|
On Leap Day 2024, CANA joined Wake Forest Law Review for an opportunity that comes around even more rarely than February 29: this gathering of thought leaders from across the death care spectrum — practitioners, reformers, lawyers, advocates, and more--to talk about the biggest legal and regulatory topics in the profession. While the Law Review hosts similar events annually, the topic varies and this happened to be a banner year to talk about changes to death care. The goal was to develop scholarly content and discussion on legal and regulatory topics in death care. This was a law symposium after all, and there are myriad legal questions related to disposition, licensure and the Funeral Rule that are in the news--and sometimes in dispute--right now. If you were unable to attend in person or via livestream, recordings are available. Additionally, the Symposium will be covered in an issue of the Wake Forest School of Law Review to be published in fall 2024. This post will be updated with a link at that time. The result of our day together was discussion that covered familiar, progressive ideas from the profession and new takeaways from reformers. Panelists were passionate about their topics and outright disagreements surfaced around licensure and the Funeral Rule, but arguments were thoughtfully presented and everyone walked away with new ideas to consider. When I reflect on my involvement in planning, implementing and presenting during the Symposium, I have identified a number of takeaways and questions that remain. Let this post capture some of those thoughts and questions and serve as fodder for future conversation. New Ideas with Roots in Funeral HistoryCaitlin Doughty served as keynote for the day and delivered a thoughtful, researched and provocative assessment the historical influences on the modern funeral profession and death-curious community. I won’t attempt to summarize her talk in this post, but invite you to listen to the recording. Funeral service as a profession has been stubbornly gendered since its inception in the mid-19th century. It was a gentleman’s profession that embraced embalming and developed many of the customs and traditions that endure today. There are parallels to this trend within cremation and in cemeteries. Women have always been involved in caring for the dead but, until the last decade, were not well represented among licensed funeral directors and embalmers or cemeterians. Professional funeral service is now proving attractive to women, and 80% of new mortuary school and funeral service graduates are female in 2024. When other professions, such as teaching, nursing, librarianship, have shifted from largely male to female, it has resulted in lower pay or a diminished reputation for its workers. There is such a shortage of licensed funeral directors currently that this seems unlikely, but the danger remains. While many women enter traditional mortuary science and funeral service programs as students, many others are carving out their own studies and career paths to become death doulas, death educators and consumer advocates. Both groups cite leaders like Caitlin as inspiration to embrace caring for the dead. Can we, the death care profession, provide a career path for new workers to satisfy their impulse to serve? Irreconcilable Differences?It may seem counterintuitive that funeral reformers and practitioners could find common ground, but we managed to agree on some of the elements of the most controversial topics in death care today. LicensureIf the more than 700 registered attendees at Wake Forest, in the overflow room, and on the livestream are any indication, interest in death care is high. But for those uninterested or unwilling to pursue licensure as a funeral director, a career path is unclear. The profession is experiencing a workforce crisis. The number of new licensed funeral directors has held steady in recent years, but that is not sufficient to offset the higher rate of baby boomer retirees and, eventually, baby boomer deaths. Discussions during the Symposium continued to come back to this topic and raised questions without easy answers: Do licensure requirements accommodate and support new dispositions and prevent scandals? The assertion from reformers and some practitioners is that the current licensure system is somehow insufficient. That is true in the sense that criminals will ignore laws and regulations and will be stopped by enforcement. Licensure and regulations are designed to create barriers to entry and establish minimum levels of competency to promote public safety. This is a good thing, but also up for interpretation as to the nature of those barriers and definitions of competency. The path to legalization of new forms of disposition is not without barriers, but our elected officials and the funeral profession are responding positively to consumer interest in greener technologies. End-of-life care is evolving, are current laws and regulations keeping up? Why is it important for a funeral director to also be an embalmer? Roughly half the states allow one license for a funeral director and another for embalmers, while the other half require a funeral director to do both to be licensed. There was much discussion about “ready to embalm” requirements, including licensure and specific equipment at establishments, that raise costs for businesses and barriers for entry into the profession for new professionals and companies. For businesses that offer embalming, it is logical to have trained professionals, equipment and facilities to offer embalming. But for an increasing number of establishments that offer direct cremation, arrangements only, or new forms of disposition, a requirement to be “ready to embalm” runs counter to their business practice. Is discussing funeral arrangements a matter of free speech or consumer protection? A recent lawsuit in California and an ongoing lawsuit in Indiana raise this question in relation to the work of death doulas. The answer will impact the future of licensure for funeral professionals as well as career paths for death doulas and educators. Can we find a way to meet in the middle and identify a path to employment for death curious people, as well as future funeral directors, embalmers and cemeterians? MoneyThe Funeral Consumers Alliance is dedicated to lowering costs for consumers and is promoting revision of the Funeral Rule to require online price posting to accomplish this goal. Funeral professionals remember that the original Funeral Rule implementation did not result in lower prices overall and any new Rule provisions or revisions are unlikely to do so. More regulation increases costs for businesses that are passed on to consumers. Funeral poverty is a real concern and any funeral home owner knows it as they scan through their accounts receivable. What the public does not see is the common practice of discounting services for veterans, children or victims of crimes. There is a larger societal pattern of lower savings and insufficient financial planning for retirement or common emergencies. If the average American does not have enough savings or credit to pay for a flat tire, will they be able to afford an unexpected death? This reality was on full display during the pandemic and resulted in discussions about potential solutions. Dr. Victoria Haneman shared the strongest argument for preplanning and preneed that I have ever heard from industry insurance and trust professionals. Dr. Haneman then laid out her proposed solutions, centered around income tax and savings incentives. These ideas are fascinating and likely to proceed as expansions of HSA or 529 plans. The NFDA has sponsored a bill that has attracted bipartisan support and would represent progress toward addressing saving for end of life expenses. Public TrustThe Funeral Consumers Alliance asserts that the funeral profession is routinely harming consumers via high prices and confusing practices; however, there is little evidence of harm as measured by complaint volume at federal or state level or via consumer ratings and feedback. Funeral practitioners have high online ratings and positive customer feedback survey results. The FTC identified funeral related complaints to be #29 in their rankings. This disparity in experiences is hard to reconcile, but we must continue to communicate the value of funeral service. Posting pricing online is a current practice for many practitioners, and may soon be required by the Federal Trade Commission. No one likes to be told what to do or how to run their businesses, hence the opposition to this requirement. Practitioners also know that price posting alone will not increase consumer knowledge about end-of-life planning or make it easier. Price is only part of the equation. When choosing an end-of-life provider (death doula or funeral director), trust is more important than price for most people. Scandals also undermine public trust. Caitlin Doughty asserted that additional regulation and licensure may not be the solution to avoid scandals as we have seen in recent headlines. She suggested instead that inspections and enforcement of existing laws could have a major impact. This dynamic is playing out in Colorado right now with a bill to require individual licensure under consideration as well as debate around funding enforcement of existing laws. What did we leave out?Whether intentionally or not, we lacked the time to cover every death care topic of interest to participants. We didn’t convene a panel about green burial or burial conservation trusts. These are established dispositions with fewer outstanding legal questions. But are they viable dispositions in the future of death care? Absolutely! We hoped that the Symposium would bring together passionate people who don’t often interact and we succeeded. The following is a quote one participant shared in the post-event evaluation: I appreciate that the symposium included views from the legal community and what I would consider funeral-adjacent professions and organizations. We don't often get outside of ourselves at funeral association classes/meetings/conventions, and at times risk becoming echo chambers. But there is so much to learn from other professional communities. I would love to hear more from professionals in the hospitality industry (which I consider funeral-adjacent, as we're all just creating experiences) that have been transformative in their businesses and industries. Thank you, for creating the opportunity to hear new--and sometimes uncomfortable--perspectives through this symposium. I share this hope that these conversations continue and we satisfy our mutual interests to advance death and end of life care. The Wake Forest Law Review is a student-run organization that publishes five issues annually. The Law Review also sponsors symposia. In 2024, the Symposium arranged their Spring Symposium on The Future of Death Care in America. Through the publication of articles, notes, comments, and empirical legal studies, the Law Review provides the profession with timely evaluations of current problems in the law and serves students as a valuable educational tool. The Spring Symposium was livestreamed and recordings can be watched here with students' publications on the topics to be published soon. When planning the Symposium, we knew that Professor Terry Brock’s research and work on abandoned cemeteries did not fit neatly in the theme, however we recognized that if we don’t study our history, we are destined to repeat it. Look for a future post to CANA's Cremation Logs blog on this interesting and important research.
It’s no secret that consumers’ increasing preference for cremation is impacting the traditional funeral home business model. Because cremation services generally produce lower revenue, many funeral home owners are expanding their product and service offerings. Others are discovering ways to serve the needs of new groups within their communities. As reported in IBISWorld industry research and echoed in the NFDA’s 2023 Cremation & Burial Report, “It is predicted that funeral homes will continue to expand their array of extra services offered to families; increase their focus on niche markets to differentiate themselves; and draw attention to their value-added services, such as … serving groups with diverse cultural and religious preferences.” Cultural differences play a significant role in funeral practices and the better we understand the religious and cultural diversity of our communities, the greater our opportunity to serve those groups. Ask yourself three questions:
Breaking Down Cultural BarriersIn Orange County California, for example, our team at The Omega Society was contacted by a writer for Orange Network, the monthly magazine of the Orange County Japanese American Association. She was writing a story to inform and educate the local Japanese American community to the range of funeral, cremation and burial options available from the Society. Southern California has the largest Japanese American population in North America, and many adhere to the beliefs of the Shinto faith. She told us that in Shintoism, terminal illness, dying and death are considered “impure,” making frank discussions of death and dying very difficult and even taboo. The result is a population with insufficient knowledge of end-of-life care and local resources available to assist them when the need arises. Our Omega Society location leader met with this writer for a tour of our facility and a wide-ranging discussion that included cremation options, costs, the advantages of prepayment, and options for the disposition of cremated remains. The resulting article did a great deal to shed light on this important subject and positioned The Omega Society as a caring local partner with professionals ready to assist the Japanese American community with all their funeral service needs. This is just one example of funeral professionals who are filling unmet community needs and finding new markets among diverse cultural and religious communities. Honoring Buddhist TraditionsLocated 20 miles southeast of downtown Portland, the city of Happy Valley is one of the most diverse communities in Oregon, including an Asian population of more than 22 percent. Our Sunnyside Funeral, Cremation and Memorial Gardens has worked with local Buddhist temples to serve this community for more than 60 years. Buddhists believe that the soul is reincarnated; death is not the end, so it is not to be dreaded. Most Buddhist societies cremate their dead to purify and free the soul, and aid in the attainment of enlightenment -- just as The Buddha himself was cremated. “Although funeral services can vary by sect of Buddhism, all are beautiful, meaningful celebrations in which family members participate over a two-day period,” said Sunnyside General Manager Samantha Haxton. “Common elements include an invocation to the Buddha, offerings of food and flowers, readings from Buddhist scriptures and a procession of monks. The body of the deceased is transported to our crematory on the second day, where final chanting and praying proceed cremation. Some of our Buddhist families choose to permanently memorialize their loved ones by interring their cremated remains at their temple and many are placed at our Sunnyside Memorial Garden near a large statue of Buddha.” Cultural and Religious Diversity are Here to StayThe shift in ethnicities and increasingly diverse funeral traditions across the United States will only accelerate in the years ahead. As funeral professionals, it’s our job to learn about and appreciate the different cultures and religions present in our communities. We need to make ourselves seen in these communities and let families know we are available and ready to serve them in keeping with their unique customs and rituals surrounding death and mourning. Do your research, build relationships and provide support to all segments of your changing community. Differentiating your funeral home by understanding and accommodating all types of funerals will help you remain a trusted service leader for years to come. May is designated as Asian American, Native Hawaiian and Pacific Islander Heritage Month to recognize the contributions and influence of these communities to the history, culture, and achievements of the United States. As experts in service, expanding your cultural IQ not only helps you serve your whole community, but also helps them to know they can turn to you when in need. Take some time in May – and year-round – to learn something new about the people in your community.
Catch CANA and Foundation Partners this week at 2024 ICCFA Annual Convention & Expo for a session on Preserving Celebrations in a Cremation-Centric World!
This post excerpted from an article of the same title published in The Cremationist volume 60, issue 1. Members can read the full article by logging in to the CANA website. Not a member yet? See the full benefits of membership and join today!
Many of us now spend a huge segment of every day engaging with the world online. As we conduct business—paying invoices, registering for continuing education, renewing subscriptions and memberships—we expect our experience to be as hassle-free and user-friendly as possible. CANA wants to honor your valuable time. To that end, we recently updated our association management software, which includes a new content management system to support a new website. Staff transferred previously existing website content to the new software and updated the design for a fresh look and feel. Most CANA members visit the CANA website once in a while to accomplish a specific task--pay a dues invoice, purchase a class or look for another CANA member. CANA’s website looks new, but still supports the content you have come to rely on while bringing you an enhanced functionality. Want a few tips on how to proceed? CANA staff created this handy guide to help you save time and support your activity as you cruise the new website. I want to…Take a CANA Course
Don’t have a profile already? Our new site makes it quick and easy to create one! Fill out this form with your information. If you are on the staff of a CANA Member organization, you may experience a brief delay while we connect you to your company. Once your profile is ready, you can login to register for your online or in-person course. Renew Our MembershipThank you for being a CANA Member! If you recently got your notice to renew, you have a few options:
If you prefer, you’re always welcome to turn to the post office and renew by check — our address hasn’t changed! Pay an InvoiceReceived a membership dues invoice? Follow the directions above to place it in your “done” pile. Have a different type of invoice? As detailed above, follow the directions to log in to our website and you’ll find a full transaction history. To log in, you’ll first need to reset your password. The quickest method is to find the the email you got from us and follow that link. Or you can enter your email address here to rest your password. (You can always contact CANA if you get tripped up along the way.) Once you’ve logged in successfully, check your profile and your company’s profile to locate the invoice you want to pay. You can also keep this card on file for future invoices. Find a CANA MemberIn the market for a new product or service? Need to make a trade call and want to work with a CANA Member? Look no further than the CANA Member Directory! Every membership includes a listing in our directory so consumers and colleagues can always find your business. Supplier Members are featured in the CANA Marketplace, organized by categories for the variety of services they provide. Try searching by keyword, location, or business category to find a company that specializes in a particular product or service. Funeral homes, cemeteries, crematories and other practitioners are featured in the Member Directory. You can search by state to locate a business in a particular region. Try a search if you want to see what businesses hold a membership in your area. Be sure to look for your own listing, too, to make sure the information we have for you puts your best foot forward. Need to make an update? Look to the next section. Update Our Directory ListingOne of the primary reasons motivating this software upgrade is to ensure that you’ll have better control and more options when deciding how your company appears in our directory. Not only will you find it easier to keep your information up-to-date, but you can also designate a general phone or email address for consumers on your company profile in addition to the direct phone or email information in your individual profile. There is a whole range of new features you can add to your company profile, including links to your social channels, pictures of your facility, an introductory video, and a new form that makes it easy for consumers to contact your business directly. In addition to your new and improved directory listing capabilities, you also have complete control over the employees tied to your member record, meaning you can easily add new staff or mark them as inactive. These employees will hear from CANA directly and can log in to register for a course, but you get to decide what level of control they should have over your company listing. Get started by logging in. The first time you log in, you’ll need to reset your password. Follow the email you got from us (easiest) or enter your email address here to kick it off (easy) — if you get stuck, contact CANA to get help (always). Once you’ve logged in, you can update your information and then Switch Profiles to update your company information. We’ve got your back, which means we’ll double-check any changes that come through. Join CANA
Help with the RolloutDid you get stuck? Meet up with a bug? Run aground on a 404? We want to hear about it! Here’s a survey where you can tell us where you encountered your issue and what happened. We’re grateful for your feedback to help us improve.
There’s a story about a Stanford business class who was given the assignment of making the greatest ROI possible on $5 in two hours, at the end of which they would make a half-hour presentation to the rest of the class. Most students tried to buy something for $5 and sell it for a little more within the two hours, making a small return. Others recognized that the $5 was really a distraction and spent their time conducting services like filling bike tires for $1 around campus. They were more successful. But the most successful group recognized that their most valuable asset was neither the $5 nor the two hours. It was the opportunity to present in front of a room of Stanford MBA students, which they sold to a local employer for hundreds of dollars – racking up a return in the thousands of percent. The point is, don’t get distracted. And definitely don’t get distracted by a dollar figure when you’re considering what you have to sell that’s of value. I’ve met funeral home owners by the score who shake their heads in frustration and say something to the effect of, “Boy, did we step in it when we positioned cremation as an alternative to the funeral. (And to memorialization, and to ceremony, and to engagement with the funeral home…).” And they’re right. But the good news is, that’s not a mistake we’re stuck with. The trick is not to get distracted. Don’t get distracted by what a family thinks they want to pay. Don’t get distracted by the phrase “direct cremation.” Don’t get distracted by conceptions of yourself as a disposal solution. Don’t get distracted. The entire concept of “direct cremation” and asking for it as an escape route from your normal offerings is not new. Jessica Mitford was encouraging her disciples to demand it 60 years ago. But there’s some encouraging data that suggests we can still stem the tide. It Was Never Really About CostMy firm has conducted more than a million dollars’ worth of research on consumer preferences on death care in the past few years. One of my favorite data points deals with expected costs of death care services. We’ve asked a huge, statistically representative sample of Americans what they would expect to pay for two things: a funeral with a burial, and a funeral with cremation. We can then average all the responses to get a sense of the general perception of cost. When you do this multiple times, in multiple decades, you get to watch how preferences evolve. Over the past ten years, the answer to the “burial” question has remained exactly the same, when adjusted for inflation, to the dollar. Remarkably, the average American expects a funeral-with-burial to cost exactly what they did a decade ago. But over that same period, Americans’ perception of the cost of a cremation has significantly outpaced inflation. In other words, the gap is closing. And we can expect it to keep closing. Because it was never really about cost. Americans’ preference for cremation is decreasingly tethered to cost. As with other low-frequency purchase decisions, like houses or cars, cost is simply all we know to ask about. We buy vegetables all the time, and therefore understand to make decisions on cost, but also on freshness, quality, organic, and so on. But we don’t plan funerals often enough to have those reference points, so we revert to the first thing we can think of. That’s why most Americans say the first question they ask if planning a funeral is how much it will cost, but only a tiny percentage of Americans say the cost is the worst thing about the funeral. The $5 is only a distraction. Don’t fall for it. Consumer-Centric InnovationHere's another key statistic: only 14% of Americans agree with the statement that, “with cremation there’s no need for a funeral, memorial service, or other form of life celebration.” Fourteen percent! To hear your average funeral pro tell it, it’s at least 50. But only one in seven Americans really sees cremation as a “way out” of the ceremony. Now, more than that, one in seven might not want their local funeral home to have anything to do with the ceremony, which is a value hurdle you need to clear. And more from there might not ever get around to dealing with Aunt Maude’s ashes, which is where your experience and leadership come into play. But it’s vital to recognize the distinction: direct cremation isn’t really what most people want. Not even close. When Apple launched the iPhone, Microsoft CEO Steve Ballmer literally laughed at them for the price tag: “…That is the most expensive phone in the world. And it doesn’t appeal to business customers because it doesn’t have a keyboard.” Ballmer failed to recognize that while the prevailing strategy of the time was to sell phones business-down, Apple flipped the model on its head by going consumer-up. Today, there’s no distinction between your “work phone” and the phone you use to scroll social media. Not only did Apple give us that customer-centric innovation, they charged a premium for it. Funeral homes and cremationists would do well to remember that message: when you give the consumer what they’re asking for, you’re providing more value and can charge more, not less. In fact, that’s a pretty solid litmus test for whether you’re actually providing value as a business. Grocery stores discount the stuff they can’t sell otherwise. Department stores discount last season’s styles. If you’re giving your customers a discount, it’s an admission that what you’re selling isn’t really the valuable thing. And they know it. You Have More To Offer Than $5So, quit being distracted. In the death care space, your disposition services are the equivalent of the Stanford students’ $5. Making money off of it is enticing, and makes logical sense, but if you step back and take stock of the situation, you might notice you have much more valuable assets than that five-dollar bill. You have a market who doesn’t understand grief, who is hurting, afraid, and burdened, and they’re walking into your business. And you know exactly what they need to heal and how to help their community do the same. It doesn’t take a Stanford MBA to notice that’s worth a lot more than a few hours’ rental of your retort.
Imagine stepping into a room filled with forward-thinking professionals eager to explore new, sustainable, and environmentally friendly options in the deathcare profession. The "Thinking Green" CANA Cremation Symposium in February promises innovation, where attendees can learn more about investing in fresh offerings, concepts, and services for their businesses. It's an exciting prospect, and the possibilities are endless. But here's the truth: having new, groundbreaking products or services in your arsenal is only half the battle. Without a well-equipped and effective sales force, those remarkable offerings risk becoming nothing more than dust-covered inventory and untapped potential. case in pointIn 2022, a certain cemetery (whose name we'll leave out of this narrative) made a noteworthy change. They observed that their top-selling urn vault was, for lack of a better word, underwhelming. It was a plastic, felt-lined, and barely-protective product, yet it was flying off the shelves, and understandably so – it came with an enticingly low price tag. In response, the cemetery decided to remove this particular urn vault from their price list entirely. They left it to the sales and service team to offer the product only in situations that warranted it, rather than featuring it in literature. It seemed like a logical step towards promoting higher-quality, more protective offerings, and a brief memo was electronically sent to the sales team to let them know that the product would no longer be found in their price book. In addition, samples of the superior vaults were added to each display unit. However, there was a critical piece missing from this equation: thorough communication and sales training. The cemetery failed to inform its sales force about WHY this change was happening and failed to equip them with the necessary tools to effectively sell these higher-quality, higher-priced alternatives. Fast forward to 2023, and the results were all too familiar. That low-cost urn vault, the same one that had been deemed insufficient in 2022, continued to reign supreme. Not a single additional unit of the superior, higher-priced urn vaults had been sold in 2023. The cemetery's well-intentioned change had gone unnoticed by the sales team, and the status quo remained unchanged. nothing sells itselfThe lesson was clear: nothing sells itself. Even when you have cutting-edge, eco-friendly, high-quality, and innovative products or services, you need a team that can effectively convey their value to your customers. As humans, we tend to gravitate towards what we know, what's comfortable, and what requires the least effort. In the absence of a compelling sales strategy, the default option often wins, regardless of its true worth. And contrary to popular belief, yes, salespeople are humans (insert chuckle here). As we look forward to the "Thinking Green" CANA Cremation Symposium, where innovative and sustainable deathcare options take center stage, let's not forget the pivotal role that a comprehensive sales program plays. A well-equipped sales force is the linchpin that transforms remarkable products and services into tangible solutions for your clients. Mark your calendars for my session at the Symposium, titled "Growing Sales: Selling with Sensitivity," scheduled for Thursday, February 15th at 8:30am. In this transformative session, we will explore an approach that seamlessly aligns sales ambitions with genuine concerns for families. Join us to discover how empathy, service, and connection can elevate your sales strategy and empower your team to present and sell innovative offerings effectively. In the world of deathcare, where innovation and sustainability take center stage, remember that nothing sells itself. It takes a dedicated and skilled sales force to showcase the true value of your offerings. Equip your team with the knowledge, skills, and motivation needed to present these innovations persuasively. Step into a transformative approach to deathcare sales. For even more insights on growing sales by selling with sensitivity, join Liza Altenburg at CANA's 2024 Cremation Symposium. There, she takes the stage to show you how to seamlessly align your sales ambitions with the genuine concerns of the families you serve. Sharpen your ability to resonate with and understand each individual's emotional landscape using a groundbreaking suite of tools. By the end of her session, you'll have mastered strategies that guide you confidently from prospecting to closing and beyond, all while nurturing deep, authentic relationships. Register to join us in Las Vegas!
In the fast-paced and ever-evolving landscape of leadership, the ability to thrive under stress is a hallmark of effective leaders. Understanding our own tendencies is a crucial first step. Leaders who are self-aware can better comprehend how their actions impact others, fostering a culture of empathy within the team. A key element in navigating stress is providing a balanced combination of support and challenge. This equilibrium liberates the team, encouraging them to push boundaries and reach their full potential. Leaders who master this delicate dance create an environment where innovation and growth flourish. The distinction between influence and power is critical for leaders striving under stress. While power relies on authority and control, influence is built on trust, respect, and collaboration. Choosing influence over positional power fosters a positive team dynamic, where each member feels valued and empowered to contribute their best. Intentionality in team development is a strategic move that pays dividends. By investing time and resources into cultivating the skills and strengths of each team member, leaders unlock untapped capacity. This not only enhances the overall effectiveness of the team but also enables achieving more with the same resources. Leaders who thrive under stress are those who embrace self-awareness, balance support and challenge, wield influence judiciously, and invest in intentional team development. This multifaceted approach not only fortifies a leader's ability to weather storms but also propels their team to unprecedented heights of success. After all, true leadership isn't just about managing under pressure but thriving and enabling others to thrive as well. The world is volatile, uncertain, complex, and ambiguous. How we navigate through that reality is important for ourselves and our teams. Janice Honeycutt Hering takes the stage at CANA’s 2024 Symposium to look at the challenges we are facing post-pandemic and the added expectations to lead well even when we don’t know the clear path forward. Participants will get key insights into their own tendencies, understand how to identify how their team members need to be led and will walk away with several tools to use immediately in their work and personal lives. See what else we have planned and register today!
Marketing flame cremation to an ecologically-conscious audience presents a unique set of challenges. These individuals are often deeply concerned about their environmental impact, and flame cremation can seem at odds with these values. However, with thoughtful strategies and a nuanced understanding of both the process and the clients’ concerns, it is possible to address these challenges ethically and effectively. At CANA's 2024 Symposium I’ll be presenting “Create a Brand for People ‘Thinking Green’” to help providers discover the ins and outs of how our two-location family-owned funeral home launched a distinct funeral service brand dedicated to sustainability. We’ll explore how this approach can not only create moral continuity for environmentally-minded families but empower all families with choice. We’ll explore ways to ensure your organization is acting with ethical integrity and avoids being accused of the dreaded “greenwashing”. We’ll also delve into language that speaks to a new generation who are likely unchurched and distrusting of the funeral industry. In the talk you’ll learn practical steps to position yourself in a way that earns genuine authority and attention in your marketplace. Today we’re going to dive into the marketing challenges facing cremation providers and ways to communicate value to an audience that may be pushing back against cremation. 1. UNDERSTAND YOUR ENVIRONMENTAL IMPACT PERCEPTION The primary challenge is the perception of the environmental impact of flame cremation. The existing impression is that traditional flame cremation is energy-intensive and releases carbon emissions, along with other pollutants. This can be a significant deterrent for those who prioritize ecological sustainability. It’s important to understand that some objections cannot be overcome, and that’s okay. Flame cremation does not have to be the answer for everyone. It is important to focus your communication toward people who will likely be receptive to it. 2. EDUCATE THE AUDIENCE Many eco-conscious individuals may not be aware of the advancements in flame cremation technology that reduce its environmental impact. If your crematory includes more efficient operating processes, filtration systems to minimize emissions, or heat recapture systems, communicating these advancements clearly and transparently is essential. 3. BALANCE TRADITION WITH SUSTAINABILITY For some, flame cremation is a traditional or cultural preference. Marketers need to respect these traditions while promoting more sustainable practices. This involves finding a balance between honoring cultural values and advocating for environmentally friendly alternatives or improvements. We never want to throw one form of disposition under the bus, because it is entirely possible that form of disposition was previously chosen by your audience, and you don’t want to make them feel uncomfortable or guilty for past choices. 4. HIGHLIGHT POSITIVE ASPECTS While flame cremation does have environmental impacts, it can be more sustainable than other options in certain contexts. For example, it requires less land space and maintenance compared to traditional burial, which can be an important consideration in land-scarce areas. There are also ecological impacts which are often overlooked, such as the raw materials sourced and consumed to produce embalming fluid, caskets, and vaults, and well as the fuel and resources necessary to transport these items, some of which can weigh upward of 3,000 pounds. 5. OFFER ALTERNATIVES Providing information about alternative options such as green burial or water cremation (alkaline hydrolysis) can be beneficial. While these alternatives may not be your primary service provided, offering them though partner providers shows a commitment to ecological values and provides choices for the people you serve. Providing access to natural organic reduction where permitted, or at least being prepared to provide factual, unbiased information about it, can also impart the willingness of your organization to discuss all disposition options, even if you don’t directly provide them all. 6. CREATE A MORE SUSTAINABLE COMPANY The overall brand image of the cremation service provider needs to reflect a genuine commitment to sustainability. This can be achieved through various means, such as using renewable energy sources in facilities, adopting eco-friendly office practices, participating in recycling programs, and engaging in community environmental initiatives. After reducing emissions as much as possible, the remaining emissions could be offset by investing in carbon offset projects. These projects might include reforestation, renewable energy projects, or community-based sustainability projects that can compensate, or partially compensate for the company’s emissions. 7. BUILD TRUST THROUGH TRANSPARENCY Being transparent about the environmental impacts and what is being done to mitigate them is crucial. Eco-conscious consumers value honesty and are more likely to engage with brands that acknowledge the complexities of their services in relation to the environment rather than pretending the complexities don’t exist. 8. COMMUNITY ENGAGEMENT AND EDUCATION Engaging with your community about death care and sustainability through educational campaigns and discussions on your blog or social media channels can help build a relationship with the eco-conscious audience. This also provides a platform to discuss the innovations and environmental aspects of flame cremation. Awareness and education can happen across digital platforms, but the most valuable place to start is in your own website. 9. MAKE YOUR WEBSITE IS YOUR FIRST IMPRESSION The biggest marketing mistake death care providers make is taking a set-it-and-forget-it approach to their website. Consumers are absolutely researching online before they make decisions, so it’s important to constantly be posing the questions; does my website accurately represent my company today, and is my website relevant to the needs of the people I’m trying to reach? 10. ADDRESS EMOTIONAL CONCERNS Finally, marketers in the death care space must always be sensitive to the emotional aspects of end-of-life services. This involves ensuring that marketing messages are respectful, honest, compassionate, and in tune with the emotional journey of someone considering a cremation option. By addressing these challenges head-on and with sensitivity, marketers can effectively communicate with an ecologically-conscious audience, providing them with the information and options they need to make informed decisions that align with their values. How do you go green? There’s no one way. Learn about the many paths to environmentally-friendly practices and explore the right solutions for your business. Join roundtable conversations, hear colleagues’ experiences, discover solutions, and return with practical takeaways that bring success for your families and your business. Head to CANA’s 2024 Green Symposium this February — register today!
People are celebrated for accomplishments in a variety of fields, for making a lasting difference, and sometimes just for having that "je ne sais quoi" that sets them apart. But when it comes to remembering someone, celebrity or not, we focus on creating an experience as special and unique as they were. In this year's post, we see how memorialization can be candlelit and private or explosive and out-of-this-world. Each experience is as unique as the life lived when it's carefully designed to commemorate what made that person important. Taking time to craft a memorial and to remember the people we care about allows us to keep them close just a while longer and demonstrate what they meant to us. After all: "The dead can survive as part of the lives of those that still live." - Kenzaburō Ōe (1935-2023) Celebrity entries appear in alphabetical order. Read to the end to see a special tribute to a mom from her sons on Mother's Day and discover how a pair of determined historians brought a Miracle to Santa Monica Boulevard. Jane Birkin DECEMBER 14, 1946 – JULY 16, 2023 Jane Mallory Birkin, OBE was a French and British actress and singer, whose controversial collaboration with Serge Gainsbourg in 1969 on the song “Je t’aime…moi non plus” catapulted her into fame and jumpstarted her career. Birkin appeared in such films as Evil Under the Sun (1982), Blow-Up (1966), and Death on the Nile (1978). In 1983 she was seated next to Hermès chief executive on a plane, and after complaining she couldn’t find a bag that suited her needs, Hermès created the now iconic leather “Birkin bag” the next year. In addition to her career as an entertainer, Birkin was also a social activist her entire life – even when it came to her namesake – and donated the royalties she received from Hermès every year to charity. Fans lined the streets outside of Saint-Roch Church to pay their respects, and Birkin’s funeral ceremony was screened for them while friends and family attended inside. Birkin’s daughters carried their mother’s casket on their shoulders while her song “Fuir le bonheur de peur qu’il ne se sauve” (“Running away from happiness lest it run away”) played. During the ceremony, Birkin’s daughter, Charlotte Gainsbourg, reflected "I see all your souls in pain without her. I can already see the void she has left in us. She is my mother, she is our mother." Birkin’s cremated remains were taken to Montparnasse Cemetery in Paris, the same cemetery in which her daughter, Kate Barry, and ex-husband, Serge Gainsbourg, are also buried. doug 2010 - NOVEMBER 28, 2023 Doug was adopted by the founder of the popular social media account WeRateDogs, Matt Nelson. Already 10 years old and suffering health and behavioral issues, Doug would have been euthanized in a shelter. Instead, he was named the CEO of the 15/10 Foundation – an organization inspired by his own story in an effort to assist dogs like him who are less likely to get adopted due to the cost of veterinary care or other unique needs. Doug earned the #1 spot in the December 1st episode of WeRateDog’s “Top 5 Dogs of the Week” after the aging canine communicated to Nelson that it was time to go. When asked if Doug should have a communal or individual pet cremation, the response was immediate: "if you didn't know, Doug HATES other dogs... He'd be so [expletive: angry] if he had to share a furnace." Despite how he reacted to other dogs, inspiring a Foundation that helps the good boys and girls that need more care to find forever homes ensures Doug's legacy will live on. In the 15/10 Foundation's farewell post, they encourage everyone: "If you ever have the opportunity to adopt a senior dog, do it. The grief is never-ending, but so is the love." michael lampton MARCH 1, 1941 – JUNE 9, 2023 Dr. Michael Logan Lampton, the first rocket scientist employed by University of California, Berkeley, worked for 54 years designing space optics and collaborating with NASA to train others on how to perform research experiments in space. In 1985 Lampton started his own software firm, Stellar Software, which sold the optical ray tracing software he developed when working with NASA. In 2015, the doctor decided to make this software free for anyone to download and use as a way of thanking the community for their many years of support. Although there were plans for Michael to make a space flight, a variety of events prevented him from doing so during his lifetime. A celebration of life was held for him at UC Berkeley in August, and a portion of his cremated remains will be sent into space in late December, along with those of 233 others. They will be attached to a satellite’s cargo bay, where they will go on to make infinite loops around the sun, allowing Michael Lampton to travel through space for eternity. milt larsen APRIL 9, 1931 – MAY 28, 2023 Highly regarded as one of the most influential figures in the history of magic, Milt Larsen co-founded The Magic Castle with his brother Bill in 1963 and served as President until his death in May 2023. The Magic Castle has become an iconic, world-renowned private club for magicians and fans alike. Prior to opening The Castle, Larsen worked as a writer for audience participation shows like Truth or Consequences. It was while working on this show that Larsen spotted the building that would become The Magic Castle from his office window. The club became so beloved by the magic community that Dai Vernon, 1968 Magician of the Year, was rumored to have had his cremated remains interred on a shelf at the castle for some time after his death. A public memorial, complete with magic and live music performances, was held at Los Angeles’s Wilshire Ebell Theatre in July, the same theatre where Larsen launched his first magic show, It’s Magic!, in 1956. The show is still running today. In September, Arlene, Larsen’s wife of 34 years, ensured he got the farewell he’d always wanted. Around 100 of Milt’s family and friends held a Viking funeral for him, an appropriately-sized sendoff for a larger-than-life personality. Milt’s cremated remains were contained in an urn made of sugar (to better dissolve in the ocean) and placed on a longboat that was then exploded to cheers from the watchers 500 feet away on the California shore. Afterwards, Arlene held a “Knowing and Loving Milt” celebration at the Magic Castle Cabaret. shane macgowan DECEMBER 25, 1957 – NOVEMBER 30, 2023 Shane Patrick Lysaght MacGowan was a British-born Irish punk musician who founded The Pogues, the famed band that infused punk with traditional Irish music, in 1982. The Pogues released four albums before ultimately letting MacGowan go in 1991 due to the many issues caused by his severe substance use disorders. The band officially reunited in 2006 and would go on to sell out live tour runs through 2009. Their most well-known song – “Fairytale of New York” – achieved quintuple platinum in 2022. Fans, friends, and family gathered to participate in MacGowan’s funeral procession despite the fact that, as his wife Victoria Mary Clarke said, “Shane hated funerals and he refused to go to them with a few rare exceptions. So it’s incredible to think that so many people want to come to his.” A variety of beloved musicians from Nick Cave to Glen Hansard performed their own moving renditions of MacGowan’s songs while a horse-drawn carriage carried his coffin through the streets of County Tipperary, Ireland, where MacGowan lived as a child. After the funeral, MacGowan was cremated and his remains were scattered over the “The Broad Majestic Shannon” River, which appeared in a song on The Pogues’ third album. KENZABURŌ ŌE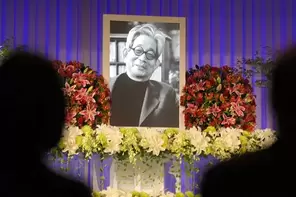 JANUARY 31, 1935 – MARCH 3, 2023 Critically acclaimed author Kenzaburō Ōe began gathering accolades for his writing when he was still a college student. He won the Akutagawa Prize in 1958 for a short story he wrote while studying French at The University of Tokyo, and the awards continued mounting throughout his life. A lifelong activist and father of three, Ōe’s works were heavily influenced both by the sociopolitical issues of his time and by his eldest son, Hikari, who was born with a herniated brain. He was awarded the Nobel Prize in 1994 for being a writer “who, with poetic force, creates an imagined world, where life and myth condense to form a disconcerting picture of the human predicament today”.Ōe’s family held a private funeral in March. In September, close to 300 people gathered for a public memorial to honor the literary giant who influenced so many. Music composed by his son Hikari was played and participants were encouraged to pay tribute with flowers. As a journalist, Ōe met with hibakusha (atomic-bomb survivors). Along with his son’s birth condition, these experiences contributed to his unique perspective of hope and despair: “Every time you stand at a crossroads of life and death, you have two universes in front of you; one loses all relation to you because you die, the other maintains its relation to you because you survive in it. Just as you would take off your clothes, you abandon the universe in which you are still alive. In other words, various universes emerge around each of us the way tree limbs and leaves branch away from the trunk.” -A Personal Matter, 1964 PAUL REUBENS AUGUST 27, 1952 – JULY 30, 2023 Paul Reubens (born Rubenfeld) was an actor and comedian most widely known for his iconic character Pee-wee Herman. Reubens successfully debuted the character in a stage show in 1981, but he didn’t garner international fame until the release of Tim Burton’s film Pee-wee’s Big Adventure in 1985. The following year, CBS launched the Saturday morning program Pee-wee’s Playhouse, which earned 12 Emmy awards over five years. Reubens had chosen to keep his cancer diagnosis private and only released a statement after his death: “Please accept my apology for not going public with what I've been facing the last six years. I have always felt a huge amount of love and respect from my friends, fans and supporters. I have loved you all so much and enjoyed making art for you.” A celebration of life was held for Reubens on what would have been his 71st birthday: August 27, 2023. Over 350 of his friends and family and fellow comedic stars showed up to share stories and songs. Guests were asked to sign postcards instead of a guest book and were offered a chance to interact with some of Reubens’ memorabilia. It was a very fitting tribute to such a whimsical and colorful personality. Reubens urn was interred at Hollywood Forever Cemetery, where his legacy continues to bring laughter and joy during film screenings of his 1985 cult classic. PAT SCHROEDER JULY 30, 1940 – MAY 13, 2023 Heralded as a trailblazer for women’s rights, Patricia Nell Scott Schroeder became the first woman elected to represent Colorado in Congress in 1972. She would go on to retain her seat in 11 subsequent elections before stepping down in 1997. Schroeder’s most recognized achievement was enacting The Family and Medical Leave Act in 1993, ensuring that Americans can take unpaid leave from work for qualified medical and family reasons. After leaving Congress she became a professor at Princeton and continued working in politics, mentoring candidates, and pursuing her lifelong advocacy for women by campaigning for Hilary Clinton in 2016, amongst other female politicians. The House of Representatives held a moment of silence for Schroeder on March 22, 2023 – the anniversary of the day Congress passed the Equal Rights Amendment process for states ratification in 1972, which Schroeder championed. In April, over 200 of Pat’s colleagues and friends attended a public memorial for her in Denver to remember her legacy. In an interview with NPR’s All Things Considered, Schroeder said “I always wanted to be cremated and made into a doorstop so I could hold a door open because basically what I want to do is hold doors open for people. And I figured that's what I was trying to do in my political career. So why not try and do it in the afterlife, too?”. Instead, Schroeder’s legislative legacy continues to prop up people in need, but her urn is among her peers at the Congressional Cemetery in Washington, D.C. tina tuner Tina Turner embodied the definition of a “rock star” – eventually being dubbed the Queen of Rock ‘n Roll. She started her career performing as a duo with her ex-husband, Ike Turner, in 1958. They disbanded in 1976, and Tina released her now iconic solo album What’s Love Got to Do with It in 1984 to critical acclaim. Tina would go onto become one of the best-selling recording artists of all time, acquiring 12 Grammys and list of honors and accolades much too long to detail here. She was a powerhouse performer on stage and also appeared in several documentaries and films, including the 1993 film based on her life. Per her wishes, details around Tina’s memorial have been largely kept private and her final resting place somewhere near and dear to her heart. Those closest to her held a memorial in Switzerland, where Turner had been residing with her husband Erwin Bach since 2013. Fans paid tribute to the artist with so many flowers lining her Swiss estate that the gates were opened to allow for everyone to be able to pay their respects. Her hometown of Brownsville, Tennessee, saw a surge of visitors after her death, and the Tina Turner Museum hosted its own twilight memorial to acknowledge what her life and work meant to so many. 2023 resting placesEDMUND GWENN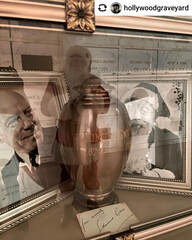 SEPTEMBER 26, 1877 - SEPTEMBER 6, 1959 Despite a career that pre-dates talking pictures, Edmund Gwenn was praised for his understanding of the medium. After entering Hollywood in 1935, he was a sought-after star of stage and screen, appearing beside Laurence Olivier in Pride and Prejudice, playing a would-be assassin in Alfred Hitchcock’s Foreign Correspondent, and portraying Santa Claus in Miracle on 34th Street, for which he won the Academy Award. After his death in 1959, his cremated remains were placed in an engraved bronze urn that was then mislaid for 64 years. The persistence of Arthur Dark, producer and host of “The Hollywood Graveyard” and Jessica Wahl, Hollywood historian, led to the recovery of his urn in March 2023 as they cataloged the vaults of the Chapel of the Pines where he was cremated. The pair organized a GoFundMe campaign to purchase a permanent place for Gwenn at Hollywood Forever Cemetery, which reached its goal in just 24 hours. On December 3, Gwenn was inurned and celebrated at the Cathedral Mausoleum before a standing-room only crowd—some in Santa hats to commemorate one of his most beloved roles. Read the full story of this journey to find Edmund Gwenn in "On the Road: Los Angeles A Christmas Miracle" published by CANA Member Kates-Boylston Publications in American Cemetery & Cremation, with thanks to them for letting us share this incredible discovery. ANNE HECHE MAY 25, 1969 - AUGUST 11, 2022 Anne Celeste Heche got her break when, at just 18 years old, she was offered a dual role in the long-running NBC soap opera Another World, for which she later won an Emmy. Her acting career spanned decades and included Donnie Brasco, Volcano, Six Days Seven Nights and John Q, before being tragically cut short when she died at the age of 53. Nine months after her death, Heche's sons decided to place her urn in Hollywood Forever Cemetery among her peers. On their first Mother’s Day without her, the family held a small private ceremony to remember what she meant to them. As her son, Homer Laffoon, said: "She was our Mom, but the kindness and the outpouring of the past few days reminded us that she also belongs to her fans, to the entertainment community, and now, to the ages." This post only captures a few of the many people we've loved and lost this year. For a list of celebrities and notable peoples' deaths and dispositions, we suggest FindAGrave.com. Today, families are seeking new, creative options for their funerals, and green values are a key influence. As the world becomes more eco-conscious, people are taking steps to do right by the environment wherever they can – and taking those values to the grave. So, your environmentally-friendly families are growing in number, but there’s no single, right way to serve them. Finding attractive options for your families and your business can leave you with a lot of questions and ideas, but not a lot of solutions and plans. The 2022 Green Funeral Conference brought together funeral professionals from across the spectrum of green funeral practice at the Sandia Resort & Casino in Albuquerque, New Mexico over September 13-15, 2022. Hosted by CANA and Passages International, more than 50 funeral professionals from across the country – from all stages of their careers, a variety of backgrounds, and representing many different businesses – attended to get ideas on incorporating green practices into their operations. Whether that’s expanding cemetery offerings, adding new disposition techniques, or considering new products, everyone left inspired to serve their communities in new ways. We’ve condensed the insights from presenters and discussion into a downloadable pdf to help you explore ways to incorporate eco-conscious values into funeral services. Here’s some highlights: putting it into practiceCANA Executive Director Barbara Kemmis led participants through an interactive presentation and discussion about common language regarding green funeral practices. Key Takeaways:
conclusionConsumers are choosing environmentally-friendly solutions for a variety of reasons: concern for the environment, enthusiasm for innovative ideas, the desire to do something new or to adhere to cultural or religious tradition going back centuries. The variety of reasons is only outnumbered by the variety of options for them to personalize their experience. As a funeral professional dedicated to serving your community where they are, you will meet people across the green spectrum. Being informed about these practices is why they chose you to offer guidance and expertise in their funeral plans. Be sure to mark your calendars for February 14-16, 2024 when we resume the green conversation at CANA’s 2024 Symposium in Las Vegas! There, CANA will bring together expert practitioners, innovative suppliers, and curious professionals to continue exploring and discovering environmentally-friendly options and how we can make a difference in our communities. Join the conversation! CANA's 2024 Cremation Symposium is your chance to get ideas for adding green options to your business. Chat with practitioners and suppliers about solutions that work and how you can put them to work for you! The event is carefully curated with sessions that generate enthusiasm for the future of funeral and cemetery service and conversations that carry over to networking, shared meals, and roundtables. See what we have planned and register to attend: The LINQ Las Vegas this February 14-16, 2024. In early 2020, a lawyer from the US Postal Service Office of Inspector General (OIG) contacted CANA. He was researching strategies to address the unidentified and misdelivered boxes of cremated remains in the possession of the United States Postal Service (USPS). After a preliminary conversation, I understood that there was a problem, but with the Annual Symposium looming in February, we agreed to continue the conversation in March 2020. Understandably, that delay lasted three years beyond the initial three-week postponement. In early 2023, different staff at the OIG launched an audit of the US postal service’s handling of cremated remains. As part of their work, they contacted CANA for recommendations from CANA members who ship a high volume of cremated remains. Not only were cremation professionals interviewed, they were also shadowed as they prepared cremated remains for mailing. The OIG Audit Report 23-018-R23 was published in July 2023 with some interesting findings and recommendations. The full report is available for download here. The report is very long and takes a lot of time to read, but the main takeaway is that the post office will focus on training mail handlers, clerks, carriers, and other staff on existing procedures without adopting recommendations to create new procedures. The United States Postal Service remains the only legal carrier for mailing human cremated remains. The OIG’s audit report provides useful insight into the internal workings and priorities of the USPS. Following is my summary of the report and CANA’s take on how this may impact cremation operations. Finding #1Noncompliance with Cremated Remains Acceptance Procedures The auditors interviewed postal workers and customers and reported finding inconsistencies in generating the Cremated Remains mailing label and affixing that label in such a way as to cover other bar codes on the box. Additionally, the interviews also indicated that the Orange Cremated Remains label was not consistently affixed on all six sides of the shipping box. OIG Recommendation #1 We recommend the Vice President Retail and Post Office Operations, develop and implement a process for reoccurring communication of Cremated Remains acceptance procedures to retail clerks nationwide. USPS Management disagreed with this Finding because the interview results were not statistically significant to indicate the scope of the problem. However, Management accepted the Recommendation, issuing the report and emphasizing the existing guidelines in staff training will address the proper handling of cremated remains. CANA’s Takeaway CANA includes the USPS guidelines for shipping cremated remains in the Crematory Operations Certification Program (CANA COCP™), and CANA members generally have a high level of knowledge and understanding of these guidelines. Despite this, operators encounter delivery delays and supply shortages of Cremated Remains Kits. This shortage may result in staff using fewer than the required six orange labels in order to stretch supplies or substituting subpar boxes or packing materials. Ensuring your business has a small supply of USPS kits on hand – and reaching out to a fellow local business when the need is urgent – can help prevent the results discussed in Finding #2. Finding #2Opportunities Exist to Improve Cremated Remains Acceptance Procedures The auditors described the risk of damage to packages containing cremated remains by the machines that process mail. Any damage can prevent recovering the contents and identifying the sender or recipient. That’s why, as of February 27, 2023, the OIG identified 452 sets of undeliverable or unidentifiable cremated remains in their Mail Recovery Center. OIG Recommendation #2 We recommend the Vice President Retail and Post Office Operations, develop and implement guidance requiring retail clerks to verify cremated remains are prepared and packaged in accordance with Postal Service policy. OIG Recommendation #3 We recommend the Vice President Retail and Post Office Operations, update the Cremated Remains acceptance procedures requiring retail clerks to place Cremated Remains packages in individual Priority Mail Express sacks at acceptance. USPS Management partially accepted this Finding again due to lack of statistically significant data, but supported Recommendation #2 with plans for staff communication and training. However, they rejected Recommendation #3 since the proper packaging and handling should prevent damage where additional handling and separation could increase the potential for delay and damage. CANA’s Takeaway There are some cremation providers who remain skeptical about or refuse to use the labels and/or cremation kits. They express concern that the labeled packages will be stolen. However, the OIG audit report describes in detail how labeled packages are processed by hand in order to limit risk of damage. With the high risk of damage during electronic sorting, CANA’s recommendation to use the USPS labels and packing materials is now backed up by facts – so use them! Also, 452 undelivered and unidentified sets of remains is shocking. In my conversations with the OIG, they described their storage facility in Atlanta with shelves containing these boxes. I answered a variety of questions to help them determine if these were human or animal remains. It looks like the USPS has the same challenge that many funeral homes have. If you have instances of lost cremated remains please consider working with the USPS to get those packages delivered. Finding #3Cremated Remains Not Monitored in Postal Facilities This was a technical finding related to the USPS processes for tracking packages and minimizing delays in delivery. OIG Recommendation #4 We recommend the Vice President Processing and Distribution, reiterate the procedures for monitoring Cremated Remains and develop a process for validating that In-Plant personnel review the Informed Visibility report daily for delayed Cremated Remains packages in accordance with policy. Management rejected this finding and the related recommendation but plans to investigate to find a more effective process for monitoring delays. CANA’s Takeaway I found this part of the report surprising: “From October 1, 2020, through September 30, 2022, the Postal Service reported 45,765 (14.6 percent) delayed Cremated Remains packages, averaging 1.4 days late.” You may not react as I did, because it may validate your experiences, but read the report for a detailed explanation. This is also the first time I have seen data on how many cremated remains are shipped. Using the data references above, during the same time period there were roughly four million cremations, meaning that approximately 313,500 cremated remains were shipped via USPS, representing almost 8% of the total cremations over those two years. Finding #4Opportunities Exist to Enhance Cremated Remains Packaging Requirements This Finding focused on shippers that use their own packaging and the problems this generated. This excerpt from the report sums it up well: “When Cremated Remains kit boxes are not readily available and take an extended period to reach customers after they place an order, customers are more likely to use their own packaging supplies.” OIG Recommendation #5 We recommend the Vice President Business Solutions, evaluate the feasibility of requiring customers to use the Cremated Remains kit boxes when shipping cremated remains and revise policy as appropriate. OIG Recommendation #6 We recommend the Vice President Business Solutions, develop a plan to ensure Cremated Remains kit boxes are readily available to customers. Management partially accepted Finding #4 but rejected Recommendation #5 since Publication 139 (pdf download) properly describes how cremated remains should be shipped. However, they accepted Recommendation #6 to make their shipping supplies more accessible to ensure ease of compliance. CANA’s Takeaway This is yet another opportunity for CANA members to share their expertise with the families they serve and pass along information about shipping or even maintain a supply of USPS cremated remains kits to keep on hand. It takes three weeks, on average, for the USPS to fulfill a request for Cremation Kits, so plan accordingly. DIY – Consumer Shipping of Cremated RemainsIn the US, the only way to ship human cremated remains (aka cremains or ashes) is by the US Postal Service, whether you are a funeral professional or a member of the public. If you are a consumer reading this article, you can ship cremated remains to share ashes among family members or send to a company to use when making keepsakes. The number one consideration for you is to use the Cremated Remains package freely available from the USPS. Otherwise you must be sure to label and pack the box securely. You can find details on preparing your shipment here, and you can always reach out to your cremation provider, or any local funeral provider, for assistance in selecting keepsakes and arranging for shipment. If you have experienced the mis-delivery or loss of shipped cremated remains, you may have options and should contact the USPS directly. Pet Cremated RemainsWhen my cat died last year, her cremated remains were sent to me via UPS (that’s the United Parcel Service, not the USPS). The cremation was conducted by a CANA member, so I reached out to find out why they used UPS rather than the USPS. Fearing the worst, I learned instead that UPS was conducting a trial-run of shipping animal cremated remains. Sure enough, only human remains, not pet, are still prohibited for shipping by UPS. InternationalWhen shipping cremated remains internationally, be cautious. The United States is one of very few countries with a postal service that handles packages. Most countries outsource parcel service to other providers such as DHL, FedEx, UPS, etc. that have policies prohibiting shipment of cremated remains. Additionally, when shipping internationally, you must get permission from the consulate to do so since each country will have their own rules about the proper handling of human remains. A number of consulates closed during the pandemic and many have yet to reopen. Shipping to countries experiencing wars and other instability is increasingly difficult. CANA highly recommends that you consult with a shipping company that has experience and resources to help you. You can learn more about those options here.
|
The Cremation Logs Blog
Cremation experts share the latest news, trends, and creative advice for industry professionals. Register or log in to subscribe and stay engaged with all things cremation. Categories
All
Archives
April 2024
|
|
