|
Learn about the common cyber threats that target small businesses that handle sensitive information and what you can do to prevent them. Suppose you run a small business that handles personal health information (PHI), personally identifiable information (PII), or payment card information (PCI). In that case, you need to be aware of the cybersecurity risks that you face. Cybercriminals are constantly looking for ways to steal, compromise, or destroy your data, and they often target small businesses that have fewer resources and security measures than larger organizations. The cost of a data breach for a small to midsize business (SMB) can be substantial. On average, a data breach costs an SMB around $217,000 per incident per the Garter® Top Trends in Cybersecurity for 2024. This figure includes immediate financial impacts such as legal fees, fines, and remediation costs. However, the hidden costs can be even more significant. For example, the average cost of lost business due to a data breach is $1.52 million. This loss stems from eroded customer trust and the potential exodus of clients, which can be catastrophic for businesses that rely on a loyal customer base. Additionally, operational disruptions, productivity losses, and data restoration costs add to the financial burden. For instance, downtime can cost SMBs an average of $8,000 per hour. Given these high stakes, investing in comprehensive cybersecurity measures is crucial for protecting against the costs and disruptions of a cyberattack. Common ThreatsSome of the most common cyber threats that small businesses face are:
Best PracticesTo reduce the cybersecurity risk for your small business, you should follow these best practices:
In today's digital age, the threat of a personal or business cyberattack looms over all of us. Take a proactive stance against cyber threats and learn how to identify phishing attacks and malware schemes so you will be better prepared to safeguard your data with Lee Hovermale this September.
At CANA’s 106th Annual Cremation Innovation Convention, Lee will present on Cybersecurity Awareness: Recognizing a Threat, and Protecting Your Data. This session will empower you with information you can use to navigate the online world securely and protect yourself and your company. See what else we have planned and register to join Lee in Chicago this September: cremationassociation.org/CANA24
During the multiple heat-related illness cases relating to the United States Postal Service (USPS), the Occupational Safety and Health Administration (OSHA) was able to establish extreme heat being a major workplace hazard. However, the agency neglected to provide effective abatement techniques in the case. Due to this, the Occupational Safety and Health Administration Review Commission (OSHRC) supported the decision made by the administrative law judge to vacate citations in all but one case. The CasesThese citations were related to seven employees working during the summer of 2016 in five cities. Every letter carrier experienced illness when they were out delivering mail in the extreme heat and had to get medical treatment. OSHA claimed that six of these workers became ill due to excessive heat. Five citations were filed against USPS for these alleged violations. The Administrative Law Judge (ALJ) vacated the five citations after finding that OSHA neglected to prove the workplace conditions were hazardous and that effective and feasible measures were accessible to abate the conditions. In four cases, the OSHRC agreed the agency established that the extreme heat conditions posed a hazard for the workers under the general duty clause but found the abatement suggestions OSHA made for the hazardous conditions for these cases fell short. For the fifth one, the OSHRC found that USPS indeed neglected to offer proper heat-related illness training to the supervisors. Therefore, this case was remanded for additional review. OSHA Failing to Prove Effective Abatement MeasuresAccording to OSHA, the USPS was in violation of the general duty clause as it failed to implement a proper program to manage exposure to extreme heat. Thus, OSHA suggested the following measures:
However, the USPS proved that it was already following most of these measures or was already in the process of implementing them. Employers Must Establish Heat Illness Prevention Plans With Proper TrainingThis recent incident highlights the significance of a detailed heat illness prevention plan. Employers must not only have a written plan implemented but also provide sufficient training to their workers. Based on guidance provided by OSHA, supervisors must be trained to:
Aside from this, the guidance also recommends employers create a heat illness prevention plan that:
Training must be provided to workers to spot stages and signs of heat illness, steps to report them, provide appropriate first aid when needed, and understand how and when to get emergency medical assistance. This post, excerpted with approval from The Federal Regulatory Review published in August 2023, is provided by Regulatory Support Services, Inc. for informational purposes only. Nothing contained in this publication should be construed as legal advice. It is always recommended that you consult your legal counsel for legal advice specific to your business.
CANA members receive a 10% discount on annual contract for OSHA and other training, services, and guidance from Paul Harris and Regulatory Support Services. Not a member? Consider joining your business to access tools, techniques, statistics, and advice to help you understand how to grow the range of services and products you can offer, ensuring your business is a good fit for every member of your community – only $495!
Disasters happen, often without warning, and businesses must be prepared to deal with them. A natural or manmade catastrophe could threaten your employees or customers and shut down or interrupt your operations for an indeterminate period of time. While no one wants to think about a catastrophic event impacting their workplace, planning for various disasters is the best way to be prepared to respond if they do happen. EMERGENCY ACTION PLAN REQUIREMENTSThe Occupational Safety and Health Administration (OSHA) mandates that virtually all employers have an emergency action plan, which details the actions that employers and employees will take during a variety of emergency situations. Employers with multiple sites must have a dedicated plan for each location. For companies with more than 10 employees, the plan must be in writing and, at a minimum, it must include several elements, including a means for reporting fires and other emergencies, evacuation procedures and emergency escape route assignments, a system to account for all employees after an evacuation, and a plan for securing rescue and medical assistance. DEVELOPING A PLANInvolve managers and staff members in developing a plan, which should begin with brainstorming what disasters could potentially impact your workplace. What if a fire tears through your offices, or an active shooter is threatening your employees? Besides fire and violence, potential disasters include hurricanes, floods, tornadoes, earthquakes, toxic gas releases, chemical spills, explosions, and civil disturbances. Once you have identified potential emergencies, consider how they would affect your workers and your workplace and how you would respond. ALERTING EMPLOYEES AND OTHERS OF AN EMERGENCYA fire is the most common type of emergency for which employers must prepare. The emergency action plan must detail how employees will be alerted to a fire or other emergency so that they can evacuate or take other actions. In addition to alarms, which should have both a sound and visual element, companies could use an emergency communications system such as a public address system or portable radio unit to provide additional information. Employees must also be trained in how to report emergencies, both to other employees and to fire, medical, and rescue services. EVACUATING OR TAKING OTHER ACTIONDetail the conditions under which evacuating, sheltering in place, or another action would be necessary. Include in the plan a clear chain of command listing who is authorized to order the action and who is responsible for leading and coordinating the process. Evacuation procedures include routes and exits, and they should be posted where they are easily accessible to all employees. The plan should detail which employees, if any, will remain in the building to shut down critical operations, and when they should abandon the operation and evacuate themselves. Designate a meeting spot or other systems in place to account for everyone after the evacuation. Back-up copies of essential company documents, such as accounting and legal documents, as well as employees’ emergency contact lists, should be stored in a secure location. WHAT TYPE OF TRAINING DO EMPLOYEES NEED?Employees should be educated about the threats and hazards that could occur in your workplace, and they need to be trained in their individual roles and responsibilities in an emergency. Training should be repeated at least annually, and new employees should be brought up to speed in the procedures soon after hire. If there are changes to the workplace that impact your plan – for instance, a redesign of the layout or the introduction of new hazardous materials – the plan should be altered, and employees retrained accordingly. Most people find it difficult to think clearly and logically in a crisis. A well-considered plan to guide their actions can go a long way in keeping them safe. Sometimes it feels like we can’t go a day without hearing about a wildfire, flood, or shooting. The tumult of the last few years has reinforced the need to prepare for the unexpected. CANA Members can rely on the expertise found in their member benefits to ensure they’re up-to-date with OSHA requirements, have standardized procedures in the business, and are covered when something happens. Then, if tragedy strikes, you have a plan in place to respond. Not a member yet? Consider joining for just $495 so your business has access to these valuable resources and everything CANA has to offer. CANA Members also receive 30-minute complimentary consultation each month with CANA Legal Counsel Lara Price. Want to learn more? Lara will be on site of CANA's 104th Cremation Innovation Convention in Atlanta next week. Register to join us: goCANA.org/CANA22.
As 2022 begins, there continue to be evolving demands competing for your time and energy. The last two years have seen some significant changes and developments in many areas of the industry and the laws which govern it. As with the beginning of every new year, it remains important to refresh and improve our habits. It is not too late to resolve to accomplish the following risk management and legal checklist items and establish a new routine for years to come. 1. UPDATE AND REVIEW CURRENT GOVERNING LAWS AND REGULATIONS. Regardless of your role in the industry, it is important to understand the current laws and regulations that govern your work. The COVID-19 pandemic has led to the implementation of many new laws and regulations which may impact your business. Put aside the necessary time to review the federal, state, and local laws and regulations which affect your daily operations. While right to control final disposition and cremation authorization issues continue to dominate legal complaints against people and businesses in this industry, there have been many new developments in the area of labor and employment, employee safety, and non-discrimination laws which may impact your business. If you have difficulty finding the statutes and regulations governing you and your business, try searching the web sites for your state association or licensing board – they often have links available. Federal OSHA and EEOC web sites, and their state counterparts, also provide significant information and updates. 2. EDUCATE AND TRAIN STAFF ON ANY NEW LAWS OR REGULATIONS AFFECTING YOUR BUSINESS. Keeping yourself updated on new laws or regulations is just a first step. The next is to educate and train your staff and co-workers on what you have learned. Hold a “lunch and learn” with your team and give everyone the tools to succeed. Education and training are vital steps to every risk management and compliance program. 3. UPDATE YOUR FORMS TO BRING THEM INTO COMPLIANCE WITH ANY LAW CHANGES. Out of date, non-compliant forms are an easy target for regulators and plaintiffs’ attorneys alike. Confirm that your form documents include all the required notices, consents, and disclosures. Consult with an attorney if you have any questions regarding current legal requirements. 4. EDUCATE AND TRAIN STAFF ON THE CHANGES IN YOUR FORMS. Compliant forms are important, but the persons who use them every day must understand how to utilize them to the fullest. Avoid the problems caused by improperly filled out forms. If done and utilized correctly, forms often provide the best documentation in defense of legal complaints. 5. REVIEW AND UPDATE YOUR OPERATIONAL POLICIES AND PROCEDURES. Regulatory compliance is critical to a successful operation. So, too, are human resource policies, and so much more. If you need assistance in your review, CANA has partnered with Cremation Strategies & Consulting to offer a program which will help you compile operational policies and procedures customized for your business. 6. REVIEW AND UPDATE YOUR EMPLOYEE HANDBOOK (INCLUDING SOCIAL MEDIA POLICY). Employment issues are a prevalent headache across all industries and business models. Address common concerns in your employee handbook, so that everyone is on notice of the standards to which they will be held accountable, including:
7. EDUCATE AND TRAIN STAFF ON YOUR POLICIES AND PROCEDURES. Periodic training and review of operational and employment policies and procedures are critical. There cannot be compliance without your employees first understanding your expectations and standards to which they will be held accountable. 8. MEET WITH YOUR INSURANCE AGENT OR BROKER. Make sure your insurance agent or broker understands your business. Make time for these critical discussions. Do not assume that your insurance agent or broker “just knows” because he or she has worked with you in the past. Too often there are gaps in coverage discovered when you need insurance assistance or defense to a legal claim, when it is too late to put the protections you need in place. Many gaps in coverage result from your agent or broker not understanding your daily work and operations sufficiently to make sure that what you actually do is covered. Just because you have “professional liability” insurance, you have no guarantee that all of your professional services are covered. Proactive insurance strategies will serve you best. 9. MEET WITH YOUR TAX PLANNING PROFESSIONAL. Do not leave money on the table. A tax professional’s advice can add value to your business and improve its bottom line. Mitigate your tax risks and exposures prudently. 10. BUDGET FOR AND PLAN TO ATTEND MEANINGFUL CONTINUING EDUCATION OPPORTUNITIES. Take some time to think about the education and assistance which will benefit you and your business most in the upcoming year. Then, search for continuing education opportunities that will assist in meeting your goals. There are in person and online resources available to address almost any concern as an industry professional or business owner. Some jurisdictions even allow you to get your crematory operator certification online. While this might be challenging as we all face the realities of a continuing pandemic, it is important to find those educational opportunities that will provide the insight and knowledge you need for success now and in the future. Getting your new year off to a good start can jumpstart accomplishing your business’s New Year’s resolutions. Best wishes for your success in 2022! CANA Members: Your association is here to help! If you ever need these resources or anything else offered by CANA, reach out.
January 7th 2016, A date that changed my life, and quite possibly other peoples’ lives, forever. Hello, my name is Michael Dixon. I am the president and founder of Funeral Professionals Peer Support. Before I tell you why that date is so important, let’s go back a bit. I was born 57 years ago in Transcona, Manitoba to two amazing, successful parents. I was the youngest – and only – boy in a family of girls. Growing up I had a lot of things stacked against me: I was born with a serious heart defect and a stutter, and in childhood I was sexually abused. The heart defect was cured and with a lot of work my stutter was overcome, but the scars of abuse stay with you forever. I hid it well. I buried it away by playing football and baseball, and, sadly, with alcohol. Upon graduating from high school and college, I started working in the hotel industry. After almost 10 years of that, I discovered that hotels just were not for me. CALLS YOU NEVER FORGETFuneral service was always my second choice out of high school, so I decided that I would give it a try. After finishing my 40 hours observation, I felt like I belonged for the first time. I was with people who were like me: kind, compassionate, and caring. I started working for a large funeral home and I was loving it. I was a sponge: I soaked in everything I was being taught, both by new directors and seasoned directors. Some are still my role models to this day. Four years into my new profession, I began to work for a removal service that this funeral home owned. There I saw firsthand how truly cruel humans can be to each other. In a three-year period, I attended over 38 murders—scenes where people were shot, stabbed, and tortured—and some of them were just children. Car accidents, train accidents, and suicides were too numerous to mention. Some calls you will never forget, even though they happened over 20 years ago. I can still picture the Christmas gifts all over the road that came from a car that flipped over on Christmas Eve. I can remember the song that was playing on the radio at a murder scene, or the smell of blood, gas, or anti-freeze. I know I am preaching to the choir, but things like this never leave your memory. They make you turn the radio off when you hear “Welcome to the Jungle“ or take another route in order to avoid the site of that accident, suicide, or murder scene that is embedded in your memory. Otherwise you get triggered. Or you stand in the doorway of your kids’ rooms watching them because your memory just won’t let you fall asleep. When you do sleep, it’s not a sound sleep for the recommended eight hours, because death does not just happen from Monday to Friday, 8 a.m. to 5 p.m. But with all these negative things, I never wanted to leave the profession. I tried to do my job well, hiding my feelings of failure, my low self-esteem and loneliness. I always put on a brave face, using comedy and humour to hide the depression that was slowly taking over my life. I, like most people in funeral service, felt that I had no one to go to. I didn’t want to talk to my wife about what I was feeling. The people I worked with at the time did not offer a safe place to talk about your feelings. There were no organized debrief or talk-down sessions, and the ones we did have were usually at a bar with alcohol, which is not a positive healing environment. In that time, the feeling around our profession was “You knew what you were getting into.” So, like everyone else, I went ahead and did my job well. I made good work friends and worked hard, but, due to my depression, I was never myself. I was always putting on an act—which often got me in trouble at work and especially at home. I always felt that I never fit in at either place. I didn’t think of myself as a good person, especially not a good father and husband. I thought many times that everyone’s life would be better if I was not around. JANUARY 7, 2016One thing about depression, it’s a slow killer. The year 2015 should have been a great year: I had a beautiful home on a nice piece of land, my three amazing kids were successful and taking on the world; my wife was in a good job and an active, well-respective member of our community; I was in a job that I loved, and for the first time I felt loved and respected. But things were starting to unravel for me. I had terrible anxiety. I hated to be away from home, and when I was at home, I was usually in my room, cut off from everyone. I was not sleeping well, I was having terrible anxiety attacks where it felt like a heart attack—trouble catching my breath, chest pains, etc. I was using alcohol now as a crutch more than I had done in the past, using it to give me confidence to go out, to make speeches, and to meet people. A month before Christmas in 2015, I decided I’d had enough. I was tired. I was tired of going on. So, I planned this suicide attempt. I scouted out locations, bought a good insurance policy, even did a practice run. January 7th was the day. That Christmas, we went overboard on gifts and had a lot of parties. January 7th came and I got up at my normal time. I was not sad or upset. I was totally at peace. I kissed my wife goodbye, drove my son to school, and off I went, pulling into the parking lot at a park. I sat there having my last cigarette and thought “Okay, let’s do this.” I opened the car door but for some reason I could not get out of the car. I could hear this voice in my head saying “It’s okay, I got you, make that call!” and I could feel these hands on my shoulder. I started to cry because I was thinking “Who would walk my daughter down the aisle or be there for my two sons and my wife?” In my despair, I made a deal with myself. I was going to call my doctor and, if someone answered the phone, I would go for help. If I must leave a message, I would walk in the forest. The phone rang once and a nurse picked up, and I thought “When does that happen? When do you ever call your doctor and they pick up the phone?” After telling the nurse that I was suicidal, my doctor came on the phone and told me to come to his office right away. After an hour of talking, I went for tests and I was diagnosed with severe depression and PTSD. FUNERAL PROFESSIONALS PEER SUPPORTFrom that point on, I decided to not be quiet, but to be very open about my diagnosis. When I told my colleagues what I was dealing with, many of them said “Man, I am going through the same thing. I am tired, frustrated, and burnt out and I am thinking of leaving.” So, instead of staying quiet and only worrying about me, I reached out to a few friends and we decided to come together and organize the very first funeral service peer support group in the world. Ottawa Funeral Peer Support was born. Our profession finally had a place where people could meet and share their personal struggles and get the support and encouragement to get help. In January of the following year, we started to get press coverage from local newspapers, which other news outlets from across Canada picked up. We then started to get requests to do radio and TV interviews both locally and internationally. Once that happened, we started to hear from funeral directors across Canada saying “We need this in our communities. We need support.” We realized quickly that our long-term goal had to be our right now goal, and Canadian Funeral Peer Support was born. Within a year, support groups have come up in New Brunswick, Nova Scotia, not to mention Ottawa, Hamilton, and Winnipeg all in Ontario. There is also serious interest in Alberta, British Columbia, Toronto, and Windsor. Then COVID hit. Our peer support groups met in person so, when everything shut down, we had to come up with a plan to stay connected with our people. It was then decided that each group would host Zoom meetings, which opened us up to funeral professionals from around the world. We started to have people connect with us from throughout the United States as well as England, Italy, Australia, and Kenya. We started to hear from people everywhere that this is something they needed and wanted to be part of. Our management team got together and we realized we are no longer just a Canadian company. We had to go international. In February of 2021 we started an international support line for licenced and non-licenced funeral staff, along with their families. With a phone call or text, you can speak to a counselor with funeral service experience that will listen and help guide you through any issue you have—for both work or non-work-related issues. We became Funeral Professionals Peer Support (FPPS). RESPONDING TO A NEEDOne thing that has made us successful is we have always responded to a need. This year, we brought Peer Support groups into the United States. We are reaching funeral professionals from across the United States and Canada with online support meetings and educational webinars. FPPS has learned is that there is no “extra money“ from our governments for mental health care. That’s why it is now the responsibility that all businesses make positive mental health care a priority in our workplaces. It is our belief that funeral service can be the leader in the goal of a positive workplace. Stats tell the story of where we are now:
Peer Support is now being looked at and valued as a positive first step in mental health care around the world. In Canada, federal government departments are now instituting peer support groups for their employees. In Canada and the United States, first responders and the military are starting peer groups as well. Peer Support helps you meet with people that speak your language, learn from people who have been where you are, and support each other. We provide tools that are applicable to the job, make no judgement, ensure confidentiality and offer the opportunity to give back. Our groups have had speakers talk about burnout, stress, compassion fatigue, yoga, healthy eating and—my favorite—personal support animals. All valuable insight into a healthy work and home life. If you are interested in a Peer group in your community or you have any questions please visit us at www.funeralpeersupport.com or call 343-961-2470. Funeral Professionals Peer Support is committed to the improvement of our brothers and sisters’ mental health. My hope is that no one else in our profession is ever sitting in a park alone in their car playing roulette with their life. CANA is honored to share Michael's story and #BeThe1To support the efforts of World Suicide Prevention Day this September 10, 2021. If you or someone you know is in crisis and considering suicide, do not wait to seek help. 988 Suicide & Crisis Lifeline (formerly known as the National Suicide Prevention Lifeline) in the US: call or text 988 (or chat) Crisis Services Canada: 1-833-456-4566 (or text 45645) If you or someone you know is struggling with mental health, reach out to these support programs: Funeral Professionals Peer Support Warmline international: 1-613-917-8057 (call or text) SAMHSA in the US: 1-800-662-HELP (4357) Wellness Together in Canada: 1-866-585-0445 If you would like to join Michael and other funeral professionals for a peer support session, CANA and FPPS are hosting a meeting on Tuesday, September 21, 2021 at 8pm ET / 7pm CT / 5pm PT and every third Tuesday each month. These meetings are open to all funeral service professionals in any stage of their career and any role in funeral service. No need to register, simply visit goCANA.org/peersupport to join the Zoom gathering.
Bereavement professionals such as funeral directors, embalmers, cemetery workers, crematorium operators, and their support staff may regularly engage with diverse, potentially psychologically traumatic events. These exposures can lead to a variety of mental health injuries, including post-traumatic stress disorder, major depressive disorder, panic disorder, and alcohol use disorder. Recent research has provided important information about those experiences, such as the scope of the challenges, the potential impacts on mental health, factors impacting health, and some of the opportunities to help protect mental health and provide support. Dr. R. Nicholas Carleton, a professor of psychology at the University of Regina and a registered clinical psychologist in Saskatchewan, introduced his discussion on challenges, strategies, and coping by emphasizing that it was really an introduction to mental health. MENTAL HEALTH EXISTS ON A CONTINUUM“There’s a long-standing notion that we are either mentally healthy or mentally unhealthy and none of the data bears that out,” Dr. Carleton explained. “It’s simply not the case. Most of us, throughout the course of a day—and certainly throughout the courses of weeks or months on end—we shift along a continuum from healthy, to having reactions, to possibly being injured, to being ill or meeting diagnostic criteria for one or more mental health disorders. And this is normal.” Odds are that people probably experience changes in their mental health throughout the entire day. Dr. Carleton described a scenario where someone wakes up in the morning and everything is fine and that’s terrific, only to move on and have somebody cut them off in traffic, and for a few minutes, they might be reacting—might even be “injured” for a few moments—but they recover very quickly and then they’re at work and moving on with their day. environmental backdropRight now, all of us are sharing a massive significant environmental variable that’s impacting our mental health—and that’s COVID-19. The impact of the pandemic is underlying all of the other things that impact us, including our biology. If we’re sick, if we have a flu, if we have a cold, that impacts our mental health. If we’re healthy and we’re exercising regularly, we’re active, that impacts our mental health and our mental health impacts our physical health as well. If we’re not feeling very happy about something, if we’re worried, if we’re depressed or down, that has a reflection in our physical capacities. We also see those same kinds of challenges with respect to our social environment. If everything is going well with our friends and our family and we’re regularly engaged, that also serves a protective function so that we’re more likely to feel physically healthy and we’re also more likely to feel psychologically healthy. Our biology, our psychology, and our social environment all come together on an overlapping Venn diagram that sits on top of our environmental stressors. it's not weaknessDr. Carleton informed listeners that it’s also important to remember that mental health has nothing to do with inherent weakness. “We have no evidence that says that there’s one gene or one feeling or one thought or one behavior or one experience that is solely responsible for our mental health or mental state. And certainly not for having difficulties with mental health,” he said. “When we talk about people who are having difficulties with mental health in most cases it’s a function of high stress or chronic strain or physical exhaustion and maladaptive coping all coming together to challenge an individual’s experience.” He pointed out that anyone can develop symptoms, saying, “At the end of the day, even the most resilient of us is still human. We still experience all kinds of highs and lows in our lives.” DEATHCARE AND MENTAL STRAINMoving on to talk about potentially psychologically traumatic events that might apply specifically to some of the work that deathcare professionals perform, Dr. Carleton spoke of experiencing, witnessing, or learning about something potentially injurious to a close relative or a friend that may cause mental health injury. He said that other potential events include repeated exposures to distressing details of significant threats such as exposure to war, threatened or actual physical assault or sexual violence, kidnapping, hostage-taking, torture, and mechanisms of severe physical injuries, like motor vehicle accidents and industrial accidents. “You’re exposed to these things because if someone dies as the function of one of these events, the last responder is you and so you are exposed to these on a regular basis,” he said. “As a species humans are generally resilient and adaptable. So even these kinds of events, when we’re exposed to them, we can bounce back, we can recover. Most stressors—even repeated exposures to these kinds of events—are not typically overwhelming. But you have to remember that our experience of whether something is overwhelming is influenced by our biology, our psychology, and our social environment, as well as what’s happening behind the scenes in our broader environmental variables.” Dr. Carleton was talking specifically about events that are potentially psychologically traumatic. He said that the most common thing we think of is post-traumatic stress disorder (PTSD) when we think about a mental health injury. PTSD can be one thing that happens following exposure to one or more potentially psychologically traumatic events where we don’t bounce back, where we aren’t able to be as resilient in that moment because of any number of things that have come together. It’s a mental health injury for which there are effective treatments that can provide symptom relief for a great many people and it’s one of the disorders that can follow exposure to the kinds of traumatic events Dr. Carleton listed. It’s also not the only mental health injury or disorder. Major depressive disorder is actually more common, even among people exposed to these ongoing potentially psychologically traumatic events. “There are also difficulties with substance abuse and dependence disorder,” Dr. Carleton explained. “You’re taking the substance for longer than you expected. You’re taking the substance in order to avoid or manage symptoms that you’re having or to change your emotional status. The problem isn’t necessarily volume. It can be the amount that someone’s consuming. But more often than not, the challenge can be that one drink might be too many and ten might not necessarily mean there’s a problem. It depends on how you’re using and what you’re using for. And if you’re using as a function of trying to manage other symptoms, that’s a good indicator that you can probably benefit from some additional support. It’s not the only indicator, but it’s certainly one of them.” Dr. Carleton underscored that only licensed qualified experienced persons can and should diagnose disorders or imply diagnosis. “Dr. Google gets us part of the way there in some cases, but that’s not super reliable,” he said. “If you’re looking for help with mental health or you’re concerned about your mental health, you want to talk to a registered, licensed, evidence-based mental health care provider who can provide you with information about where you’re at and possible solutions to get you to where you’d like to be.” SYMPTOMS AND WARNING SIGNSDr. Carleton turned to discussing some of the urgent warning signs and symptoms. First, he pointed out that if any symptom lasts longer than a week, at that point it’s a warning sign that your symptoms may benefit from some intervention, particularly difficulties with falling or staying asleep, intrusions, numbing, changes in your behavior, or sudden increases in substance use. Those are also potentially urgent warning signs and symptoms. Suicidality, homicidality, violence, or sudden dramatic increases in substance use should all be taken as urgent warning signs where it’s time to get in to see somebody soon. “It doesn’t mean necessarily that we need to call 911, although that is a possibility,” Dr. Carleton said. “It does mean that help is needed sooner rather than later.” HOW CAN MANAGERS AND COLLEAGUES SPOT SIGNS OF BURNOUT AND ENCOURAGE PEOPLE TO SEEK HELP? According to Dr. Carleton, the more open you keep communications, that peer connection, can help. But if you identify big behavior changes—someone normally jovial now lashes out, as an example—it’s a good indication that you should check in with them. The more engaged you are with your team with regular communication, the better positioned you are to support them. mental health is a journey“What can you do? Well, I think first and foremost it’s important to keep in mind that mental health is a journey, not a destination,” Dr. Carleton advised. “It’s not something you check off as a tick box because you did it well today, any more than physical health is.” He encourages deathcare professionals to monitor both their physical and their mental health. “We have tools that we make publicly and freely and anonymously available on our website for our public safety personnel, and those tools might be beneficial for you as well,” he offered. “They allow you to compare your responses to the general population, and, in doing so, you get immediate anonymous feedback that you can use to see where you are sitting relative to everybody else.” Because changing mental health requires culture change because of stigma and misinformation, it’s extremely difficult and takes a long time to accomplish. Dr. Carleton believes it’s important that we all pay attention to the idea that mental health is something we’re trying to change at a population level, but he pointed out that for people who are regularly exposed to potentially psychologically traumatic events, they may very well be forced to engage with culture change more directly than everybody else. He encouraged listeners to engage in ongoing monitoring regularly and get help sooner rather than later. self-careWhat can we do in addition to the monitoring? The doctor advised people to look to their social support. “Talk about your experiences. Not necessarily about the details of what happened in your job and specific day, but how you’re feeling and what else you’re doing in order to manage those feelings. If you’re having difficulties with the symptoms we’ve discussed, talk to family or friends. Make sure that you keep a regular diary so that you can watch what changes for you that supports or undermines your mental health.” “As cliche as this sounds—and it sounds cliche in part because we all keep saying it—engaging in regular healthy behaviors enhances your coping ability and helps to maintain your mental health,” he continued. “So, exercising regularly, even light exercise: simple walks, getting outdoors, 20 minutes. Any exercise at all tends to be beneficial as long as it’s regular.” Dr. Carleton added that people should watch what they eat. Eating healthy is important because the highs and lows of sugar affect your biology, which impacts your mental health as well. Substance use and misuse is much more problematic and a much more slippery slope than most people realize. If, for example, you’re using alcohol to manage your emotions, that’s a good indication that there’s a better set of skills you can access to manage those emotions. He also emphasized that, where possible, it was important to maintain routines, even in the face of COVID-19. “The more routines that you can build in, probably the better off you’re going to be, as long as those routines include strict work-life balance where possible,” Dr. Carleton said. “As a professor, I can tell you that the boundaries between my work and my life are permeable at times. They’re permeable most of the time, but it’s important to try and manage those separations because that’s what’s helping to protect and sustain your mental health. So making sure that you’re managing that is an important part of living an ongoing happy, healthy career.” Last but not least, Dr. Carleton addressed early evidence-based interventions. “Evidence-based interventions are evidence-based for a reason. It’s because they’re helpful. It’s because they’re beneficial and there’s proof, there’s research that says that they work.” He spoke of the importance of finding the right type of practitioner to offer those interventions. “Psychologists is a protected term. So is psychiatrist. But counselor, therapist, and healer are not protected, which means that anyone can take them—and there is a lot of variability among them. That doesn’t mean there’s not good counselors, therapists, and healers. It’s just that there are a lot fewer restrictions on those names and titles than there are on things like psychologist or psychiatrist. So I recommend you demand registered and licensed, experienced, evidence-based, empirically-supported mental health care (which is a mouthful!), but you can find that from colleges, registered provincial associations, and registered state associations.” HOW CAN WE SUPPORT EACH OTHER IN OUR OWN GRIEF?Dr. Carleton said that grief is a unique thing and shared the work of Dr. Katherine Shear on Complicated Grief. Grief is not something that’s clearly defined—you don’t have clear phases or end-point. Grief can last an entire lifetime, ebbing and flowing throughout, and in many cases it does. Grief in and of itself isn’t a problem, it’s not something to cure since it’s part of the human experience. If grief is leading to difficulties with destructive behaviors or debilitating, interfering with your job, then maybe seek help to better manage the symptoms of grief from an evidence-based professional. But grief is part of the human experience. While it’s not a pleasant emotion, it does also remind us to value all of the things we have right now because of the things we’ve lost before. With shorter days, family obligations, and a job that doesn’t recognize the change in seasons, the holidays can be the biggest strain on our profession. Combine that with a global pandemic and a surge in cases and taking care of yourself and your colleagues is more important than ever. With that in mind, Funeral Professionals Peer Support (FPPS) and CANA came together in mid-December of 2020 to help deathcare professionals gather the tools needed to keep working by offering a free webinar with expert presenters who shared strategies to address the challenges faced on the front lines during the winter months. CANA’s President W. Scott Smith addressed his experiences with the high number of COVID-19 cases in Texas. Dr. R. Nicholas Carleton, an expert on mental health on the front lines, highlighted strategies to identify problematic symptoms, suggested coping skills to help, and provided recommendations for engaging professional supports when needed. Visit goCANA.org/webinars to view a free, on-demand version of the complete webinar. Now, CANA and FPPS are coming together again to host a peer support meeting for deathcare professionals of all roles and experiences. Learn more about this meeting and mark June 22, 2021 on your calendar for this valuable meeting.
Funeral professionals have a challenging job under normal circumstances; these are not normal circumstances. Covid-19 has simply turned the world upside down. As a psychologist who works with funeral homes and also works in one, I want to offer several suggestions for dealing with the additional stress created by the current epidemic. Many of these ideas come from my work on the Finding Resilience program sponsored by Homesteaders. You can download free materials here. Professionals in a wide variety of fields consider it a badge of honor to wear many hats in their business. However, I don’t know of any professionals who wear more hats than funeral directors. Within a single week, you might be expected to demonstrate knowledge of:
In the last few months, you have also had to add “remote videographer,” “social distancing expert,” “Covid-19 expert,” and “creative rituals coordinator”. Not only are all of these duties happening under significant time pressure, but also in the midst of continually changing state and local regulations. It’s no wonder that funeral directors are feeling the effects of compassion fatigue and/or burnout. Ideally it is best to make relatively small changes to reduce feelings of burnout before it becomes overwhelming. These changes may include hiring additional staff, delegating responsibilities to others, or finding a colleague to cover during much-needed time off. Funeral professionals experiencing profound burnout, anxiety or depression may seek professional help from their physician or a therapist. Hopefully, you may only need a few “course adjustments” to keep you on a productive, lower-stress path. Here are my suggestions for reducing stress under normal circumstances as well as during the current crisis. say "no" to non-essential tasksEspecially now, there are going to be some tasks that should be postponed. There may be certain types of long-range planning or reviewing production options that are best left to another time. Even better, it is an ideal time to eliminate some of your daily and weekly tasks that don’t impact your business operations or your quality of service to families. I call this process “smart subtraction”. By reviewing your daily and weekly schedule, you may find tasks that can be eliminated, automated, or outsourced. make sleep a priorityMy work schedule has shifted. I have tried to have “fun nights” with my wife and three daughters, and I have had to adjust to extended family living with us for the last two months. This has destroyed my regular sleep schedule (and I don’t even have to go on middle-of-the-night death calls). When you add the economic stress and uncertainty to changes in daily habits, it is difficult to stay on a regular schedule and get quality sleep. Here are a few tips to help make it more likely that you can fall asleep.
write it downRecording thoughts and experiences – especially about things that inspire gratitude – can be helpful for people who routinely experience stressful workplace situations. This does not have to be a regular journal or even complete sentences. Doodling and writing short bulleted lists of your thoughts and feelings can work just as well. Don't just do something, sit therePracticing meditation and mindful activities can often seem so counter-intuitive. When my thoughts are racing around my brain at record speed, it can be difficult to be still and try to not think of anything. Thankfully, there are many different forms of mindfulness and meditation. It can help to try a meditation app or focus on slow, deep breathing. Mindfulness can also come from your religious practices such as focusing on meaningful scripture. Establishing a regular time to practice mindfulness can train your brain to transition more quickly. listen to musicI am “old school” when it comes to music. I still have a large pack of CDs in my car and I actually listen to them. I have one CD with “In Case of Spiritual Emergency” written on it. It’s a personal compilation of Eric Clapton, Paul Simon, John Hiatt, Mary Chapin Carpenter, and other favorites. I never cease to be amazed at how the right songs can lift my mood, refocus my mind, and give me a more balanced perspective. I’m not sure what should be on your “In Case of Spiritual Emergency” CD, but I encourage you to create that playlist. know you are neededI have been talking with many funeral professionals across the country and the most consistent reactions I hear include sadness. Funeral professionals are feeling sad that they are not able to provide the full range of funeral rituals and events to bereaved families. They are sad that people are dying alone. And they are sad that families are not receiving the benefits of funeral rituals including support and healing. I know you can’t do your job the way you would like, but please know that you continue to provide an invaluable service. You may not be able to give someone a hug, but your simple presence and compassion (even if expressed through a video chat) are still a vital service to grieving families. Thank you for the sacrifices of your own potential safety to serve others. Thank you for the innovative ways you have created to meet the needs of the bereaved. Do your best to care for yourself. The world needs you more than ever. Jason Troyer, PhD., specializes in helping death care professionals serve their families better. Additional resources unique to death care are available in his Finding Resilience program. Circumstances like a pandemic require extra care for yourself and your colleagues. "Stress prevention and management is critical for responders to stay well and to continue to help in the situation." Use the support resources from the CDC available by both call and text, and work together to stay healthy.
After the celebrations are over, the beginning of each new year reminds us to refresh and improve our habits. It is not too late to resolve to accomplish the following items this year and establish a new routine for years to come. 1. Update and review current government laws and regulations.Regardless of your role in the industry, it is important to understand the current laws and regulations that govern your work. Put aside the necessary time to review the federal, state, and local laws and regulations which affect your day to day operations. Right to control final disposition and cremation authorization issues dominate legal complaints against people and businesses in this industry. If you have difficulty finding the statutes and regulations, try searching the web sites for your state association or licensing board – they often have links available. CANA Members: If you need further assistance, use your legal consultation benefit and give me a call. 2. Educate and train staff on any new laws or regulations affecting your business.Keeping yourself updated on new laws or regulations is just a first step. The next is to educate and train your staff and co-workers on what you have learned. Hold a “lunch and learn” with your team and give everyone the tools to succeed. 3. Update your forms to bring them into compliance with any law changes.Out of date, non-compliant forms are an easy target for regulators and plaintiffs’ attorneys alike. Confirm that your form documents include all the required notices, consents, and disclosures. Consult with an attorney if you have any questions regarding current legal requirements. 4. Educate and train staff on the changes in your forms.Compliant forms are important, but the persons who use them every day must understand how to utilize them to the fullest. Avoid the problems caused by improperly filled out forms. If done and utilized correctly, forms often provide the best documentation in defense of legal complaints. 5. Review and update your operational policies and procedures.OSHA compliance is critical to a successful operation. So, too, are human resource policies, and so much more. If you need assistance in your review, CANA has partnered with Cremation Strategies & Consulting to offer a program which will help you compile operational policies and procedures customized for your business. Learn more here. 6. Review and update your employee handbook (including social media policy).Employment issues are a prevalent headache across all industries and business models. Address common concerns in your employee handbook, so that everyone is on notice of the standards to which they will be held accountable. Implement clear, unambiguous policies on work hours, time off, sick leave, vacation time, and dress codes. Have appropriate sexual harassment policies in place. Communicate your expectations regarding social media use and restrictions on employee posts on business matters. Make sure employees are aware that social media is not for airing of workplace grievances or complaints. CANA Members: Read up on what my office suggests for these policies as part of the Crematory Management Program. 7. Educate and train your staff on your policies and procedures.Periodic training and review of operational and employment policies and procedures are critical. There cannot be compliance without your employees first understanding your expectations and standards to which they will be held accountable. CANA Members: You can keep your standard operating procedures current and your staff informed with the Crematory Management Program and support from Cremation Strategies & Consulting. 8. Meet with your insurance agent or broker.Make sure your insurance agent or broker understands your business. Too often there are gaps in coverage discovered when you need insurance assistance or defense to a legal claim, when is too late to put the protections you need in place. Many gaps in coverage result from your agent or broker not understanding your daily work and operations sufficiently to make sure that what you actually do is covered. Just because you have “professional liability” insurance, you have no guarantee that all of your professional services are covered. Proactive insurance strategies will serve you best. CANA Members: Have you looked over CANA’s newest benefit, a professional liability insurance program for crematories? Read what makes this policy different and how it covers businesses like yours. 9. Meet with your tax planning professional.Do not leave money on the table. A tax professional’s advice can add value to your business and improve its bottom line. Mitigate your tax risks and exposures prudently. 10. Budget for and plan to attend meaningful continuing education opportunities.Take some time to think about the education and assistance which will benefit you and your business most in the upcoming year. Then, search for continuing education opportunities that will assist in meeting your goals. There are in person and online resources available to address almost any concern as an industry professional or business owner. Some jurisdictions even allow you to get your crematory operator certification online. If you attend CANA’s convention in Seattle this year, please say hello. I look forward to seeing you! CANA Members: Not sure how to get started developing a defined professional development plan for your employees? CANA Education Director Jennifer Werthman is here to help you achieve your goals – reach out any time. Getting your new year off to a good start can jumpstart accomplishing your business’s New Year’s Resolutions. Best wishes for your success in 2020! CANA Members: Your association is here to help! If you ever need these resources or anything else offered by CANA, reach out. Excerpted from The Cremationist, Vol 53, Issue 1: “First Quarter 2019 Top Ten Legal Checklist” by Lara M. Price. Members can read this article and any other advice in The Cremationist archive. Not a member? Consider joining your business to access this and all archives of The Cremationist plus the many resources referenced here to help you find solutions for all aspects of your business – only $495
When CNN’s article regarding the JAMA radiation letter first hit the CANA newsfeed on February 26, 2019, we knew immediately it would be a big deal. And yes, the story has become a many-headed hydra of confusion, concern, and misinformation, accompanied by increasingly scary rumors. We constantly field concerns from suppliers about cremated remains placed inside keepsakes, from crematory operators and embalmers about their cases, from families about their options, from regulators about all of the above, and from you — in the middle of it all — trying to serve your families, comply with regulations, and protect your staff. CANA has curated several of the most useful questions in one place to counter some of the fear, anger, and rumors. And it’s all publicly available, so please share this resource far and wide, bookmark it for later reference, come back to check for updates, and, most of all, DON’T PANIC. where it started.The radiation misinformation saga began with a research letter, titled Radiation Contamination Following Cremation of a Deceased Patient Treated With a Radiopharmaceutical and published on February 26, 2019 in the Journal of the American Medical Association (JAMA). In the letter, Dr. Nathan Yu (et. al) discussed a case study of a business in Arizona that cremated a 69-year-old man with pancreatic cancer in 2017. The deceased had been treated with an intravenous radiopharmaceutical for a pancreatic tumor and died five days later. When the medical staff became aware of the cremation, they notified the crematory and the cremation chamber, equipment, and staff were all tested for exposure to radiation. The equipment was found to have traces of contamination, as was a urine sample from one crematory operator (but it was a different isotope from the one used in the patient’s treatment). The contamination levels were below the limits set by the US Nuclear Regulatory Commission. In conclusion, because this is only one studied instance, researchers recommend further testing for more data and better understanding. CNN was the first major media source we found to bring the letter to the general public awareness. To round out the story, the network solicited the opinion of Dr. Daniel Appelbaum, chief of nuclear medicine and PET Imaging at the University of Chicago Medical Center. He said, "If there are reasonable and fairly straightforward and simple things that we can do to minimize radioactivity, why not do that?” Applebaum also acknowledged the need for better understanding and regulations that keep workers safe. In the case of crematory operators, the doctor recommends "robust enforcement of mask and gloves and handling techniques." where it went.Other media outlets picked up the story and it spread quickly, with information traveling like a game of telephone. My mother’s church group argued against cremation for spreading radiation in the community. One CANA member’s staff are expressing concerns about “the crematory operator who died from radiation” (when none have). Each of which are exaggerated concerns about what we know. Because while the case study is new, the knowledge about radiopharmaceuticals and brachytherapy is not. And the medical community is quick to reassure that there is Low Risk of Radioactive Contamination from Cremation When Proper Safety Procedures Followed. CANA is aware that these concerns and fears are rooted in a lack of awareness and understanding, so we want to provide information to help. what we know.RADIATION 101 At CANA’s second Alkaline Hydrolysis Summit, we invited Jeff Brunette, Health Physicist and Manager of Radiation Safety at the Mayo Clinic, to talk about nuclear medicine and its impact on death care. His full presentation is available as a free, on-demand webinar for you, your staff, and anyone to access anytime on CANA’s Online Learning platform, but here are some highlights:
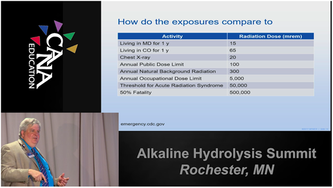
WHAT'S THE RISK? The US Nuclear Regulatory Commission has set specific levels (mentioned above) to regulate emissions and uses. In the case of cremating a body treated with nuclear medicine, the Commission and medical community agrees that the potential exposure is too low to record. Though cremation volatilizes the radiation treatment, Brunette says even extreme cases are not likely to exceed the limits set for safe exposure due to the combination of medically accepted isotopes, their half-lives, and treatment use. He explains it with an analogy: taking a daily recommended dose of aspirin is fine (around 325 mg) but taking a year’s worth at once (118,625 mg or more than three bottles) is fatal. Canadian Nuclear Safety Commission has their own rules and regulations and reviewed them extensively last year. CANA recommends their comprehensive Radiation Protection Guidelines for Safe Handling of Decedents as a great resource to learn more about the isotopes in question and safe handling procedures, even for non-Canadians. Ultimately, Brunette argues that radiation is a limited concern because the levels you will encounter on the job are small, and not very common. Your bigger concerns are the activities that your staff do every day: musculoskeletal injury from lifting, exposure to disease during embalming (HIV; Hepatitis B & C; Tuberculosis; MRSA), and exposure to harsh conditions during cremation operations (heat, noise, dust or chemicals). HOW CAN WE OPERATE SAFELY? CANA recommends asking all families for detailed medical information to properly understand and respond to potential risks. Just as you ask about the presence of pacemakers, ask about nuclear medicine treatments. Paul Harris of Regulatory Support Services encourages all funeral home, crematory, and cemetery owners to ask the pertinent questions of their families. Cause of death is the first indicator that a case is at risk for radiation therapy, but all families should be asked in the case of death unrelated to their ailment. In many cases, families may be unaware or not understand the procedures the decedent has undergone. In these cases, you may need to ask for a Health Insurance Portability and Accountability Act (HIPAA) release form (in the US, rules in Canadian provinces vary) to contact the medical provider yourself. Asking the radiologist for information on the treatment and about the specific isotope and its half-life is the best way to determine when (or if) it is safe to cremate or embalm the body. The medical community also recommends installing a simple radiation detector to quickly alert staff to the presence of radioactivity (some states require them in all morgues). Brunette recommends a pancake Geiger-Mueller counter which can be acquired cheaply (particularly if you have them left-over from the old nuclear-powered pacemaker days) and built into your case acceptance procedure. The Arizona Bureau of Radiation Control recommended a combination metal/radiation detector, such as the MetRad, which one school in considering adding to their intake process curriculum. Mostly, Brunette recommends the following steps to reduce exposure:
what we do next.The medical community should do what Drs. Yu and Applebaum say: research. Learn more about these situations so everyone can make informed choices about safety. In the long-term, this will serve us better than knee-jerk reactions and blanket rules to refuse all cases who have ever been treated. Our professional community should continue to do what you do best: serve your communities safely and compliantly. Enforce PPE, add this to your list of questions for families, do your due diligence. You should review your existing policies, processes, and procedures to ensure that you are screening for the use of radiopharmaceuticals and staff are taking proper precautions. Inform yourself and staff with basic information about diseases that could indicate potential treatments and which isotopes are used. Know who to contact with questions like your local hospital’s radiology department (or the decedent’s doctor) or regulator. Mostly, DON’T PANIC. Now that the public is aware of this issue, this is an opportunity to educate our communities and ourselves with good information from reliable sources. CANA will periodically update this post with new knowledge, so bookmark this for later. Sources of information referenced in this article:
happy new year from cana!As we lay 2017 to rest and get used to writing 2018 on our paperwork, we asked a few CANA members what resolutions they have for 2018 and each said the same thing: I don't believe in New Year's Resolutions. Instead, they strive to improve the performance and service of their company throughout the year by supporting their staff's professional development, by protecting the safety and well-being of their operators and their image, and by caring for themselves and their colleagues the same way they care for our communities everyday. These goals aren't something we can do in one day, but something we can continue to strive for throughout the year. So from our experts to you: And there's a hand, my trusty friend! And give us a hand of yours! And we'll take a deep draught of good-will For auld lang syne. We look forward to seeing all that you accomplish in 2018 and continuing our support of our members and the industry throughout the year. ERNIE HEFFNERHEFFNER FUNERAL CHAPEL & CREMATORY, INC. I don’t do New Year’s resolutions. When I’m motivated over a topic, I make a commitment and set timelines for accountability to follow through, timelines for myself included. These timelines may or may not coincide with January 1st. As much as I’m flattered to be asked to contribute to CANA’s Cremation Logs and make recommendations for staff training in the new year, I’m not even sure I know what “improving staff training” means. I also flinch at the word “training” – I think we train dogs and we educate people. Heck, for some employers, any training would be perceived as an improvement. My guiding principle, from the book Good to Great, is that you get “right people on the bus and wrong people off the bus.” If the wrong people snuck on the bus, either by acquisition of a firm, marriage to a relative or simply a wrong hire, then no amount of training will change the person. Instead, you need to do some top-grading and weed out the low performers. Great people in end-of-life care sincerely want to do all they can for a family in grief. Every year they want to enhance their skills to serve. They want to be the very best informed and most knowledgeable caregiver they can possibly be. If those are not obvious traits, than the wrong person is on the bus! Top-grading is probably an excellent resolution. The right staff will rise to the top and the opportunities for improvement will be natural. The problem is, it may start with the owner – it’s up to management to decide what talents they need and what skills they’ll teach or have others teach for them by sending staff to appropriate seminars and continuing education. In the end, the words don’t matter if there is no downside to refusing to be enlightened – make sure the right people are on the bus and get the others off. Not just January 1st, make a point of doing this continuously. larry stuart, jr.CREMATION STRATEGIES & CONSULTING Generally, I think New Year's resolutions are ridiculous. We try to solve all of our perceived problems at the stroke of midnight only to fail miserably, usually before Valentine's Day. The key to true success is to declare broad-based, realistic resolutions and work on them all year long. Baby steps, if you will. For instance, a cremationist could resolve to focus on improving three important facets of cremation operations: safety, the environment, and the public’s perception of a crematory. So, for 2018, repeat after me: "I resolve to be an even better cremationist by working to improve Operational Safety, Environmental Impact, and Public Perception regarding cremation. Working on these three goals in progressive steps will be much easier to accomplish than resolving to “never leave the crematory during the cremation,” because we know that there will be times that, sooner or later, this will happen. Then, you will feel defeated and risk scrapping the whole thing. Instead, implement the following procedures throughout the new year. Here are a few examples of things that will help to succeed with your New Year’s resolution.
mike sheedyMARKET DIRECTOR FOR MANITOBA / NORTHERN ONTARIO, SERVICE CORPORATION INTERNATIONAL Ours is a difficult job. We meet people at the worst moments of their lives and guide them through this period of initial hurt until their mother, child, grandfather, loved one is laid to rest. And then we say goodbye. They continue on their grief’s journey, we take the next call. Our journey stops, or never stops as the phone keeps ringing, without any satisfying conclusion. So in 2018, I want us all to make a New Year’s Resolution to take better care of ourselves. I need to take my own advice here. We are too often a profession in which we put others’ needs before our own. This work selects those who have so much to give and who are determined to carry on through terrible situations. We continually respond in a professional and dignified way to national tragedies, horrific accidents, or acts of violence and serve our communities while grieving ourselves while our own family awaits our return. We must take care of our mental and spiritual health and watch for warning signs in ourselves and our colleagues. We must know when it’s enough and when to reach out and ask for help. That may mean reaching out to a colleague for help with a difficult case, or for professional help to avoid or cope with a breakdown. Yes, was as death care providers can hurt too. Your network inside the profession, your social groups outside, your hobbies and passions, your family and friends all serve important functions to ground you in life when our career surrounds us is death. This year, let’s resolve to celebrate these groups, to take stock of our physical, mental and spiritual health, and to reach out to others when we need it or we feel they do. The CANA network is one of the most powerful benefits of attending a CANA event and membership with the association. CANA provides the space where cremation professionals can share important conversations with people who get you and your business. Consider connecting with CANA and other industry experts at the 2018 Cremation Symposium for topics that inspire innovative thinking. Not a member? Join your business to access this article and all archives of The Cremationist plus advice, tools, techniques, and statistics to help you understand how to increase your cremation success -- only $470. Ernie Heffner shares 40+ years of professional funeral service. He has a diverse background in the operation of end-of-life care related enterprises including funeral homes, cemeteries, a monument company, 10 funeral business relocations and 5 new replacement facility constructions. Ernie has received national recognition and has been a featured speaker on numerous occasions for a variety of state and national industry organizations, related industry organizations as well as his local public speaking engagements for community education.
Larry Stuart is a graduate of Kent State University and is a past member of the Board of Directors of the Cremation Association of North America (CANA) as Supplier Liaison. Through his experience Larry has seen first-hand the negative impact that poor crematory maintenance and improper operating procedures can bring about. Larry has spoken at numerous industry events and has conducted crematory operator training classes across North America with a mission to advance the safety of cremation facilities and their employees and to more positively impact our community and our environment. Michael Sheedy has been a funeral director for over 20 years and currently serves as President of the Board of Directors for the Cremation Association of North America (CANA) and is a member of the Ottawa District Funeral Association. In his tenure with Pinecrest Remembrance Services, he has been part of the creation of Ontario’s first full service facility with onsite visitation and receptions. |
The Cremation Logs Blog
Cremation experts share the latest news, trends, and creative advice for industry professionals. Register or log in to subscribe and stay engaged with all things cremation. Categories
All
Archives
July 2024
|
|
